All News
ACR24 Preview Podcast (11.15.2024)
ACR 2024 starts tomorrow. Here are a few previews of abstracts to be presented, along with my recommendations of sessions you don’t want to miss.
Read Article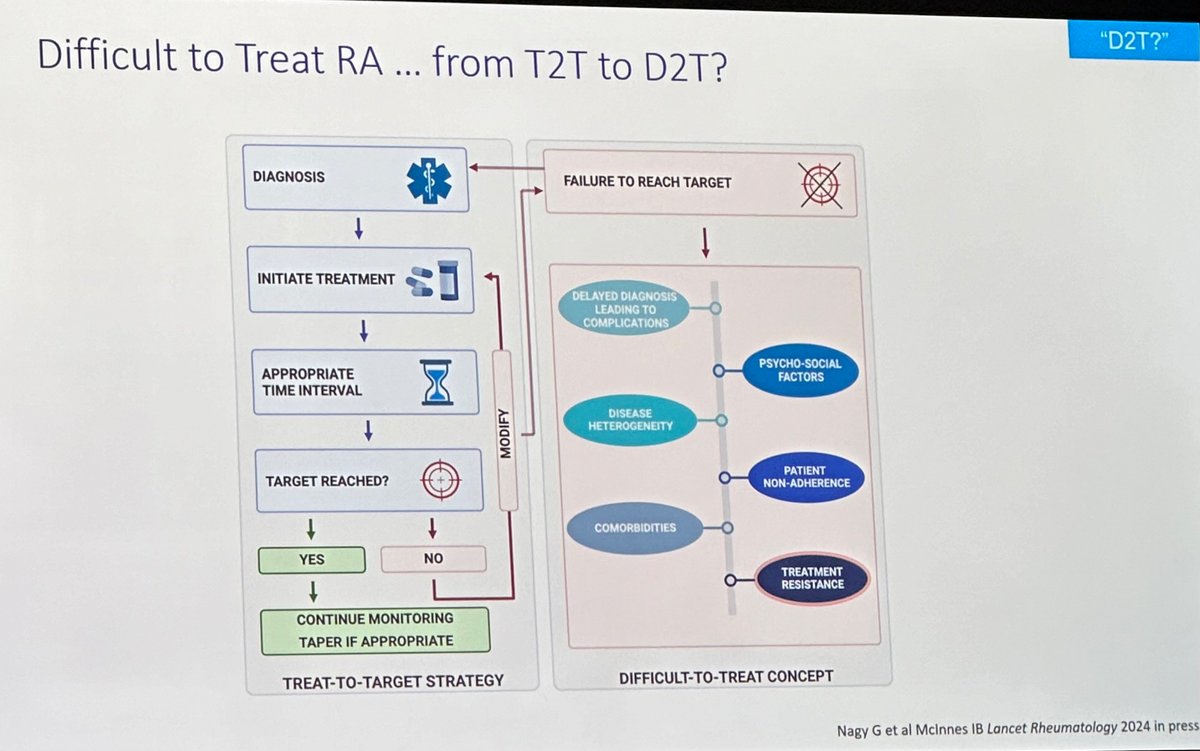
RA pearls from #ACR24 review course:
1. Remission is DRUG maintained-Ok to reduce MTX dose while on TNFi.
2. Multimorbidity=Poor outcomes, High risk for mortality.
3. Can RA be truly prevented or we are delaying the inevitable? https://t.co/111w1Myqrg
Links:
Adela Castro AdelaCastro222 ( View Tweet)
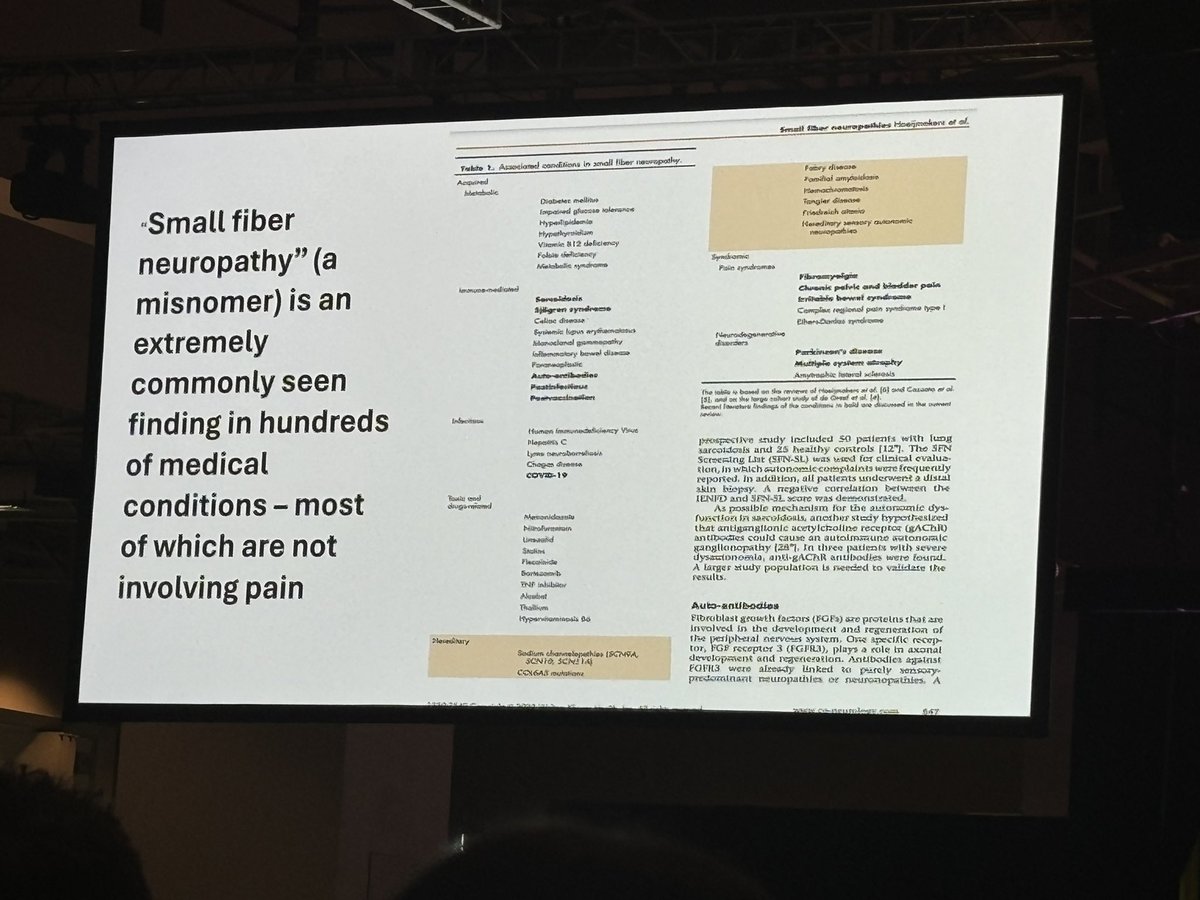
Myths by Daniel Clauw
Small fiber neuropathy - misnomer, non-specific, not worth getting a skin biopsy
Fibromyalgia is not autoimmune - it is nociplastic pain and treated differently
#ACR24 Review Course
@RheumNow https://t.co/JLyfnfMBML
Eric Dein ericdeinmd ( View Tweet)
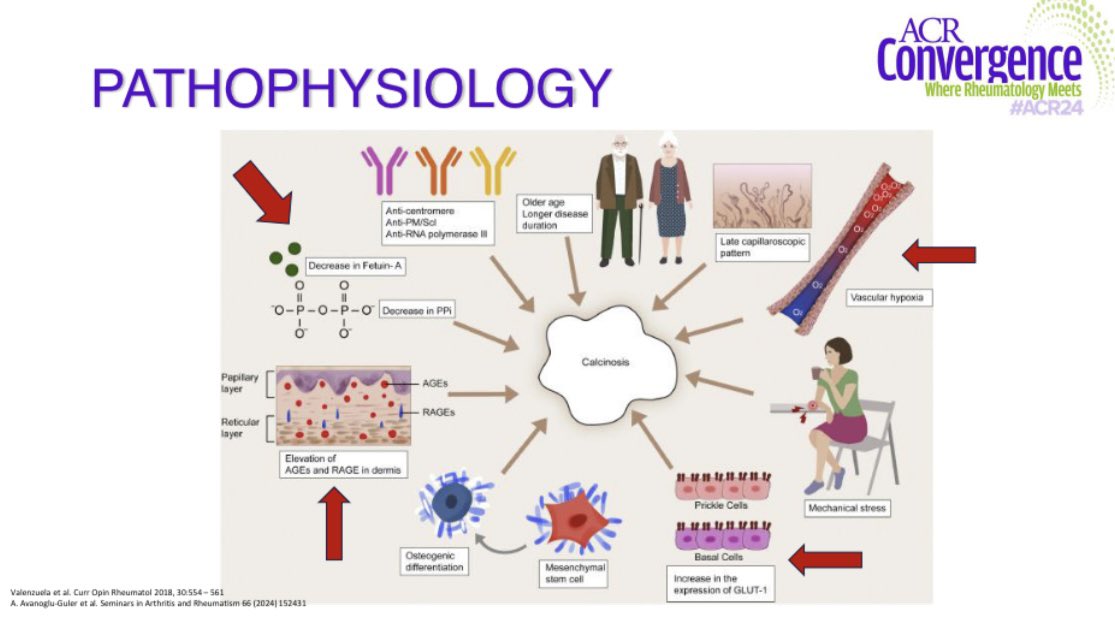
Pathophysiology of calcinosis. Antonia Valenzuela at Review Course @RheumNow #ACR24 https://t.co/gSJSa2lGXw
Antoni Chan MD (Prof) synovialjoints ( View Tweet)
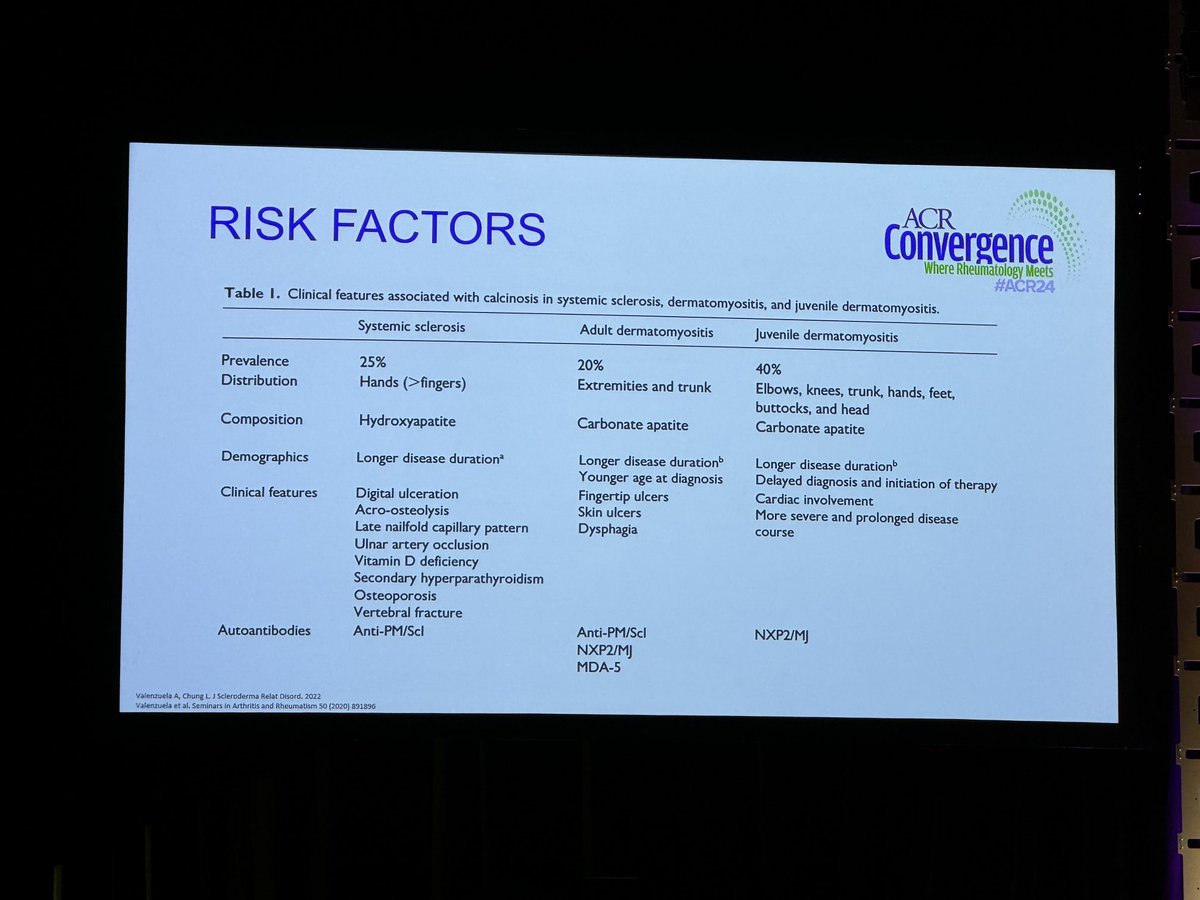
Risk factors and crystal composition of in calcinosis. In SSc - calcinosis is assc with vasculopathy, dz duration #ACR24 #ACRReview https://t.co/LJvrdVG1jg
TheDaoIndex KDAO2011 ( View Tweet)
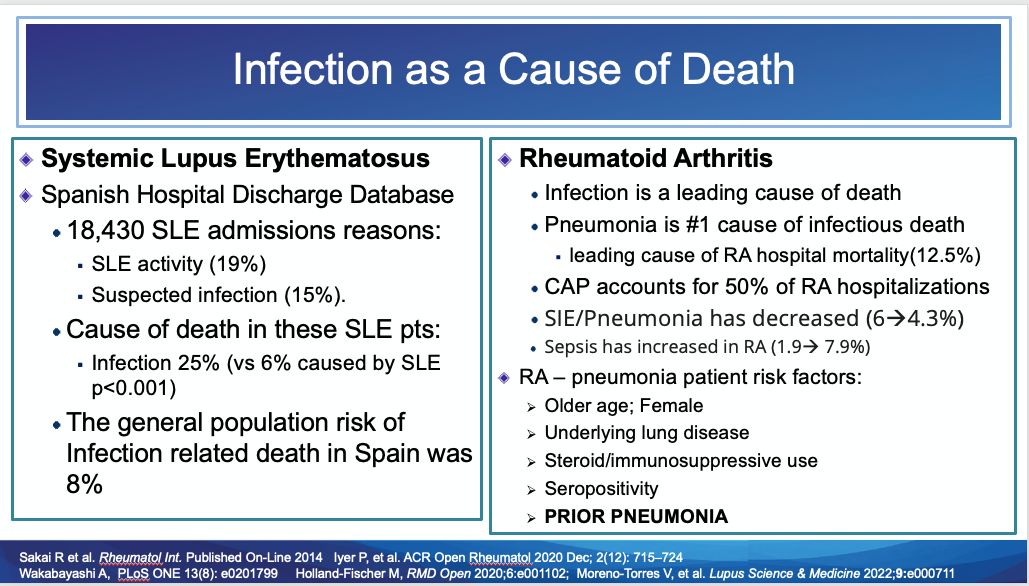
Infection as a Cause of Death
https://t.co/CwvffN7CcM https://t.co/SwSuAanuEO
Dr. John Cush RheumNow ( View Tweet)

RheumNow’s expanded coverage of the #ACR24 annual meeting is sponsored in part by Novartis. All content is chosen by RheumNow & its faculty
Dr. John Cush RheumNow ( View Tweet)
Diagnosis and Management of Kawasaki Disease
The journal Circulation has published a comprehensive overview called “Update on Diagnosis and Management of Kawasaki Disease,” summarizing data published since the 2017 American Heart Association Scientific Statement on Kawasaki… https://t.co/rS5bDneplO https://t.co/nZ0GeIQD0T
Dr. John Cush RheumNow ( View Tweet)
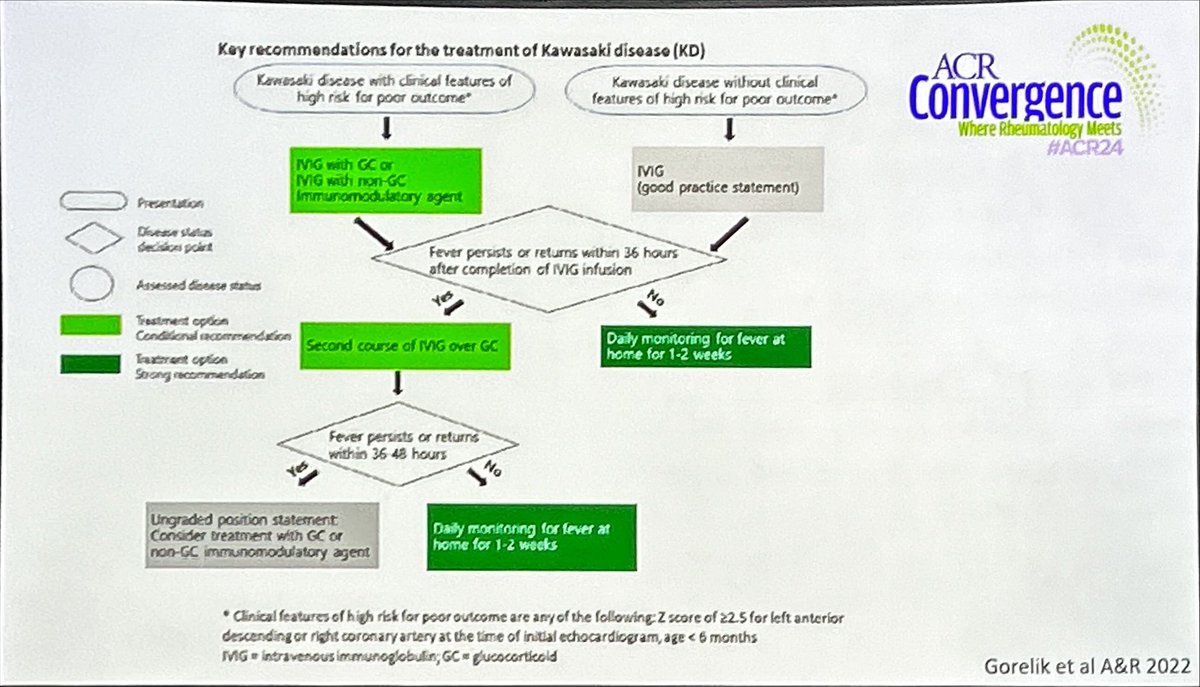
Recomendations for the management of Kawasaki’s disease. Cardiometabolic session, Bryce Binstadt @RheumNow #ACR24 https://t.co/KftwMDYzH1
Antoni Chan MD (Prof) synovialjoints ( View Tweet)

#Baricitinib in refractory #myositis?
A ‘weak’ trial design comparing #Bari to #Bari Rx started 12 weeks later
in a small N =15
neat idea but NO answer
👇
looked like 👍 it worked
BUT
this is not the #RCT design that can show differences
#ACR24 @RheumNow abst#1731
@ACRheum
Janet Pope Janetbirdope ( View Tweet)
No Increase in Cardiovascular Events with JAK Inhibitors in IBD Patients
UMKC researchers have compared the use of JAK inhibitors versus tumor necrosis factor (TNF) blockers in inflammatory bowel disease (IBD) patients, but failed to see an increase in major adverse… https://t.co/XY0UVDTAI6 https://t.co/b09FB3niNP
Dr. John Cush RheumNow ( View Tweet)
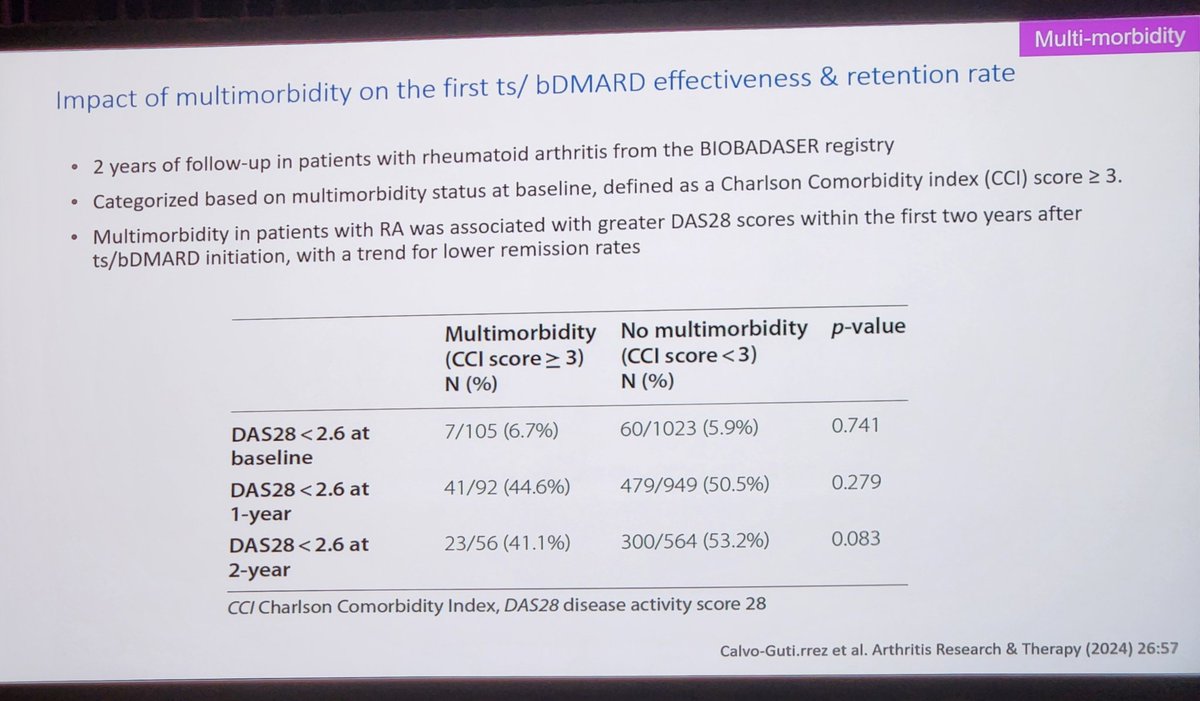
Multimorbidity reduces response to b/tsDMARDs in RA. We can make a difference by treating the whole person!
Amazing talk by Dr Iain McInned to wrap up #ACR24 #ReviewCourse.
@RheumNow https://t.co/NiaUXzt4nT
Jiha Lee JihaRheum ( View Tweet)

⭐️Top tip from Dr Laura Carbone:
🦴Rule out hypophosphatasia before starting bisphosphonate or denosumab in patients with low ALP
#ACR24 @RheumNow
Mrinalini Dey DrMiniDey ( View Tweet)
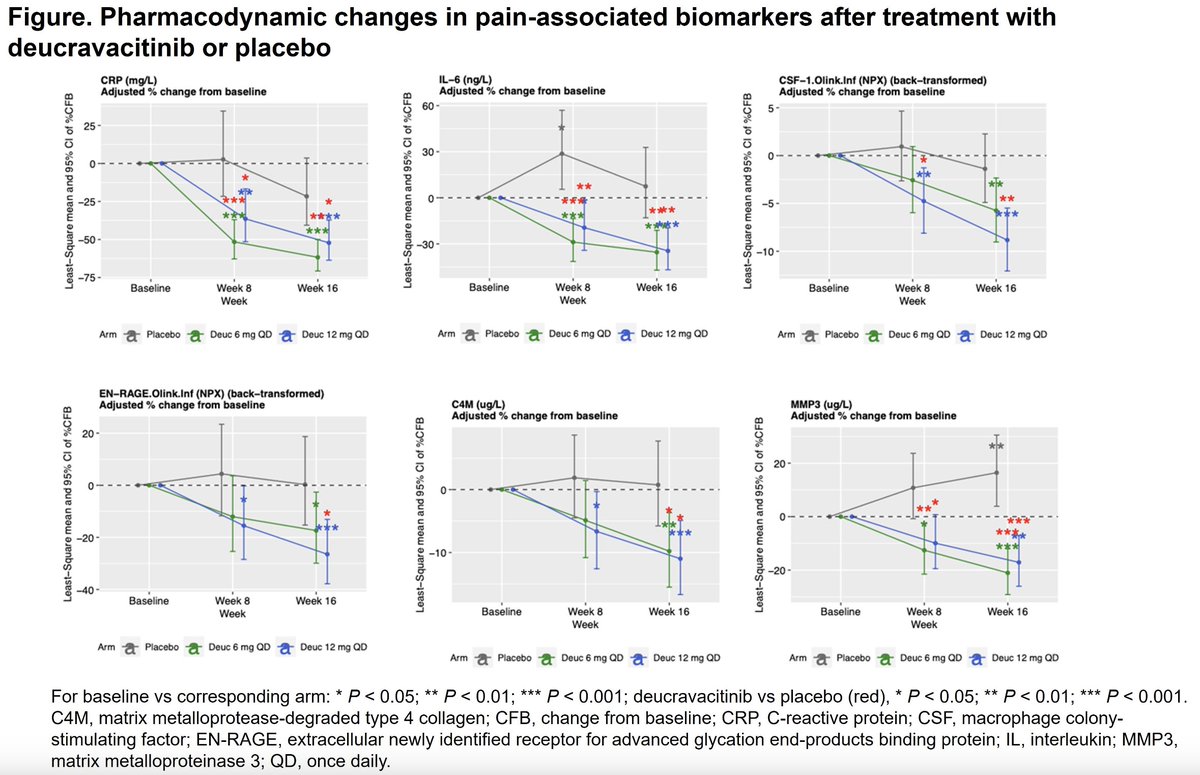
Pain in PsA = predictor of disability and QoL
TYK-2 inhibition lowered clinical pain outcomes and ALSO pain-associated biomarkers vs PBO
@RheumNow #ACR24 Abstract #2366 https://t.co/DAgmdmmTE0
Brian Jaros, MD Dr_Brian_MD ( View Tweet)
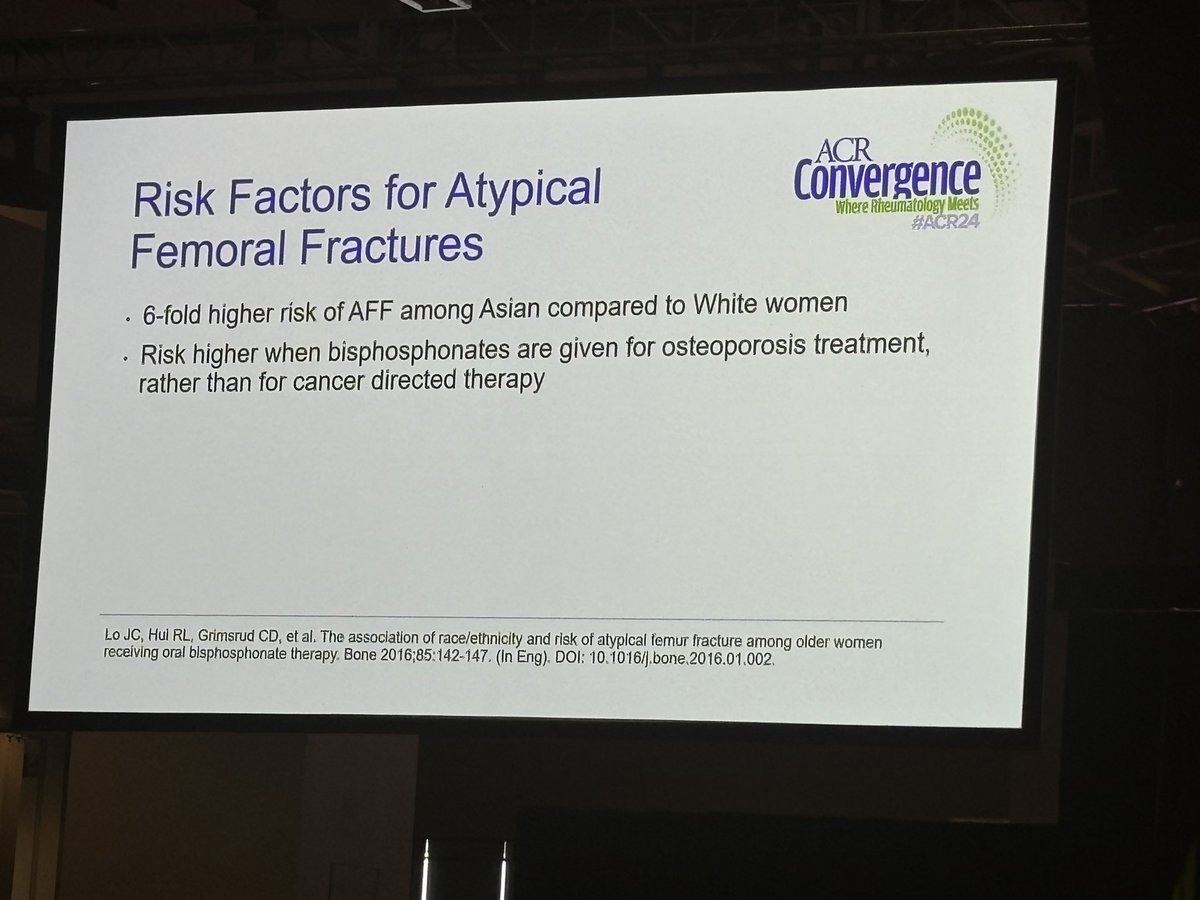
Risk for atypical femoral fracture:
🚨Asian race - 4-6x higher risk
Duration of use is greater risk than older age
Higher risk when given for osteoporosis than cancer treatment
- Compare: osteonecrosis of jaw more common with cancer Rx
#ACR24 Review Course
@RheumNow https://t.co/V8cD5QWNGp
Eric Dein ericdeinmd ( View Tweet)

Weight Loss from Anti-Obesity Medications Prevents Gout
A population based study looked at the effect of the weight loss drug, Orlistat, in obese individuals. Compared to those untreated, orlistat over 1 year was associated with significant weight loss and significantly lower… https://t.co/P1iRjtHgHV https://t.co/MoohUKGvUn
Dr. John Cush RheumNow ( View Tweet)

Study of 237 SLE pts shows mood disorders, fibromyalgia & chronic damage were major determinants of poorer Quality of life in SLE. mean SLEDAI-2k was 1.7, 29% had FM; 44% had chronic damage. https://t.co/JHzmleVMIK https://t.co/Sqk9K6oA7M
Dr. John Cush RheumNow ( View Tweet)
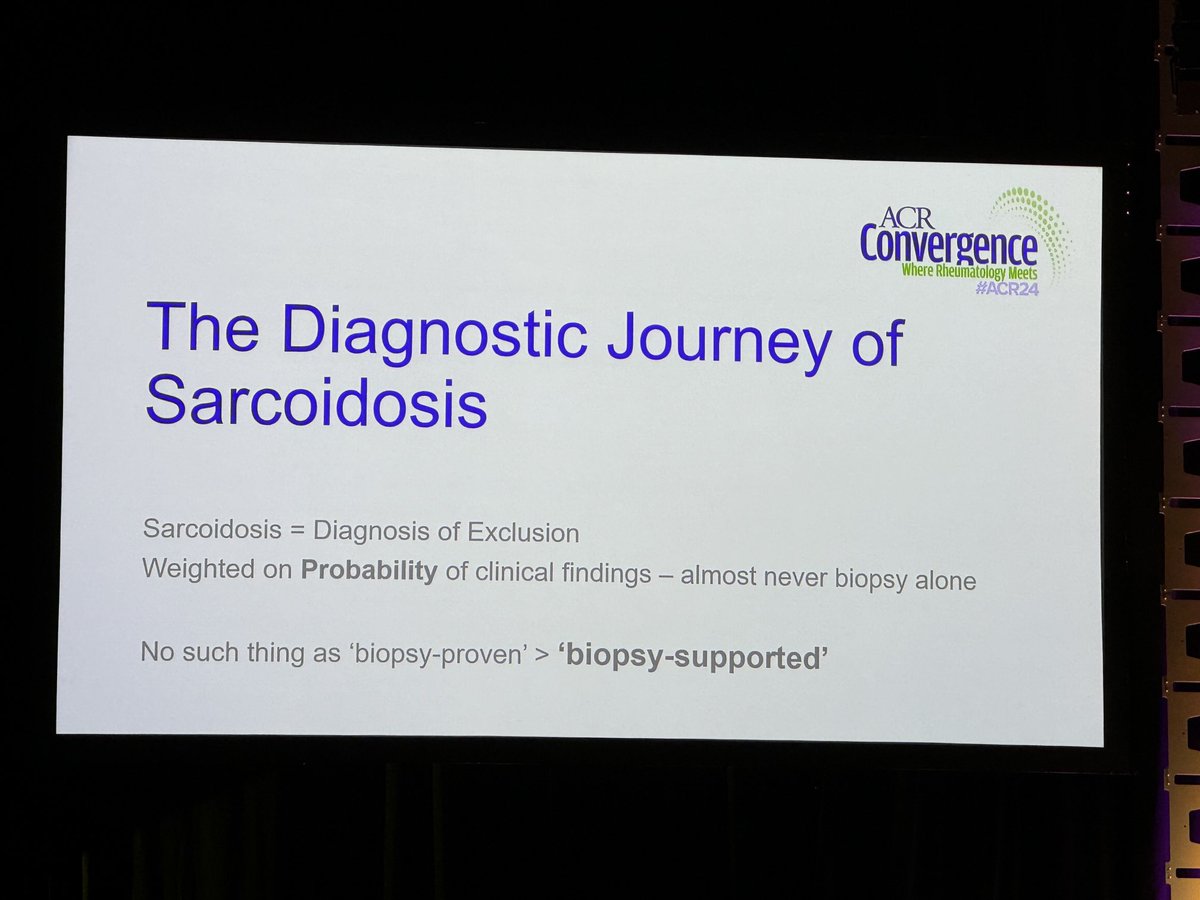
Don’t use ‘biopsy-proven’ to label sarcoidosis; use ‘biopsy supported’ as there are many causes of granulomatous inflammation. It’s happened to one of my pts who was diagnosed with “biopsy-proven” sarcoidosis - she actually had CVID with GLILD. #ACRReview #ACR24 https://t.co/it41va1K6g
TheDaoIndex KDAO2011 ( View Tweet)
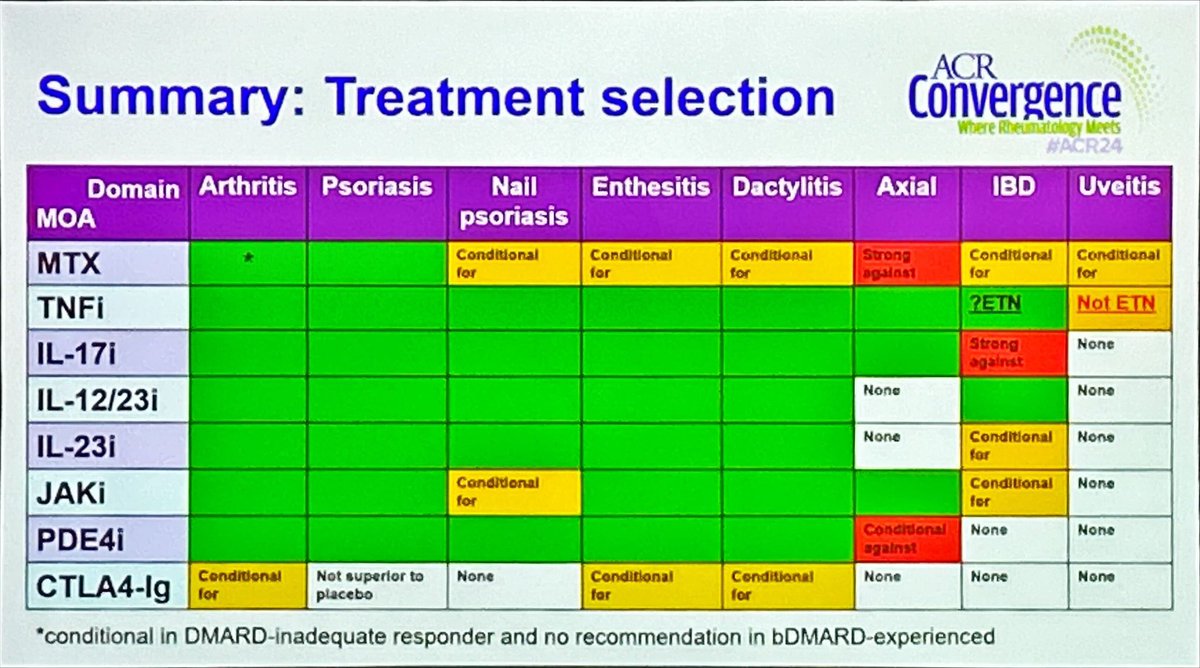
Summary of treatments in psoriatic arthritis #PsA @RheumNow #ACR24 https://t.co/EybzRCPLtA
Antoni Chan MD (Prof) synovialjoints ( View Tweet)
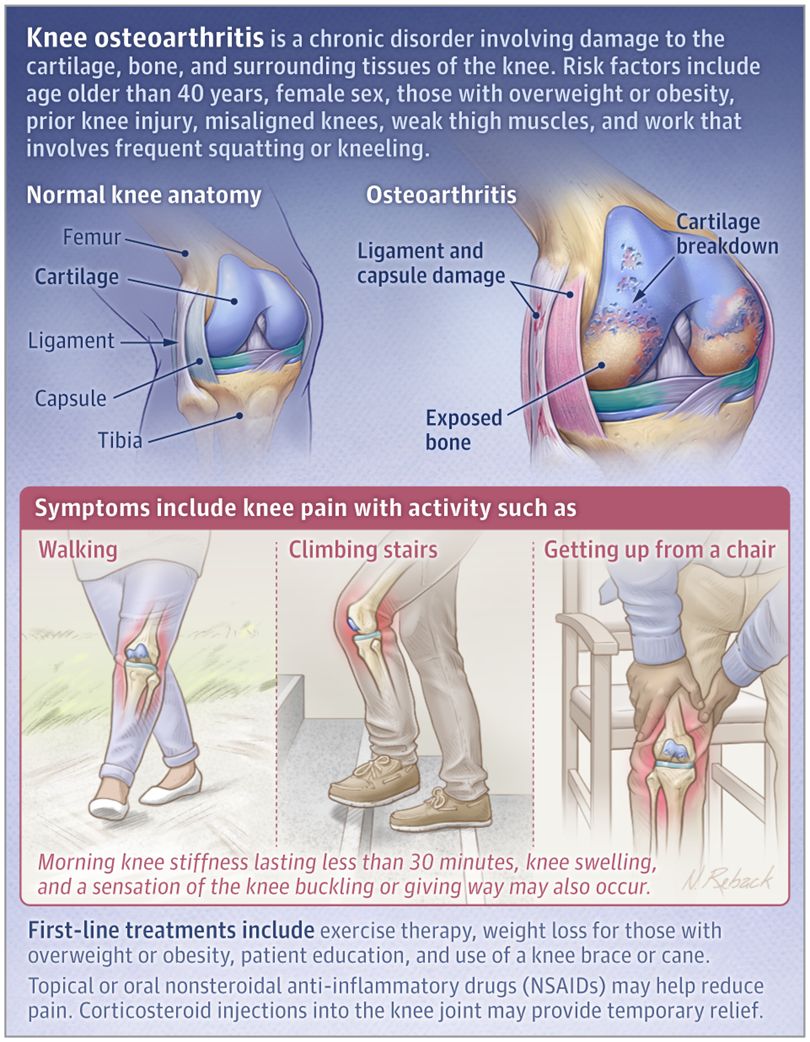
What is Osteoarthritis? A downloadable patient education page from JAMA. https://t.co/gocsQizJUh https://t.co/4bBuNUAYlR
Dr. John Cush RheumNow ( View Tweet)




