All News
Maintain Vigilance for CV Risk Postpartum in Autoimmune Diseases
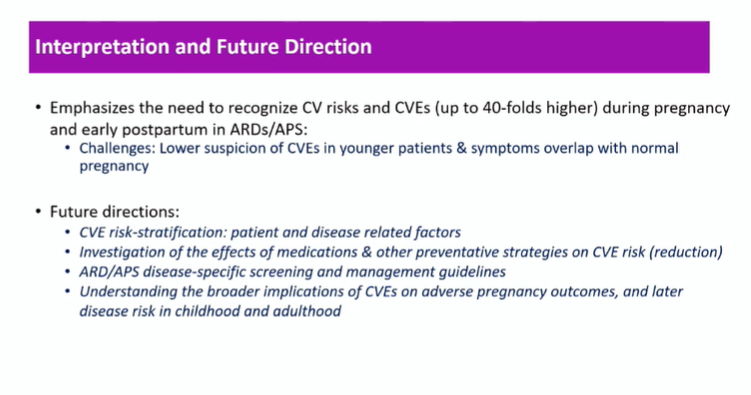
Pregnant women with autoimmune rheumatic diseases (ARDs) and antiphospholipid syndrome (APS) face significantly increased risks of cardiovascular events (CVEs). This increased risk is often attributed to ARDs, its medications or comorbidities associated with it.
Read Article#ACR BEST Abstracts from San Diego – Day 1
The RheumNow faculty reporters have been scouring the meeting for what they believe to be the best presentations from the first day at ACR 2023 in San Diego. From hundreds of online presentations, the poster floor and the plenary podium, here are some of the best abstracts from Sunday Nov. 12th. You can spot these on Twitter by looking for the (#ACRbest) hashtag.
Read Article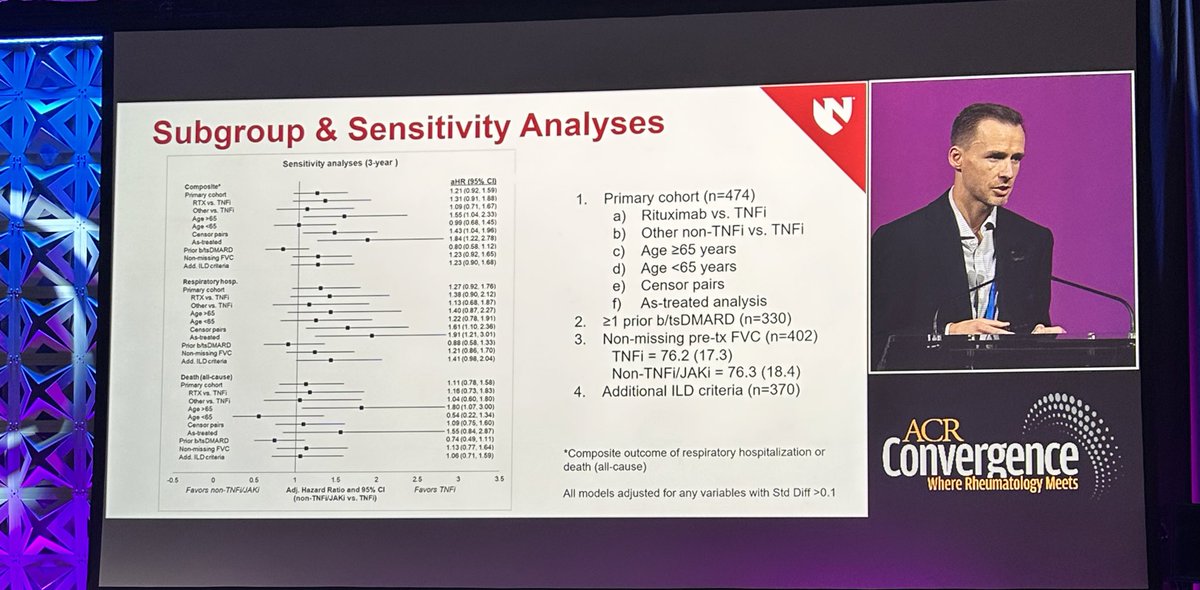
RA-ILD: the study that exonerates TNFi ?
TNFi vs. other BioDMARDs/JAK do not increase risk of death or hospitalization over 1 and 3 yrs follow up.
No subgroups stand out
VHA cohort, 50% smokers
No info on ILD patterns or disease trajectory
ABST1582 @RheumNow #ACR23 https://t.co/frv16oRLqv
Aurelie Najm ( View Tweet)

Lovering et al. Synergestic effect of RA and CVD on dementia risk. 35% increased risk RA, 89% increased risk RA+CVD. Abstr#1628 #ACR23 @RheumNow https://t.co/Brj8XrG2o4
Richard Conway ( View Tweet)
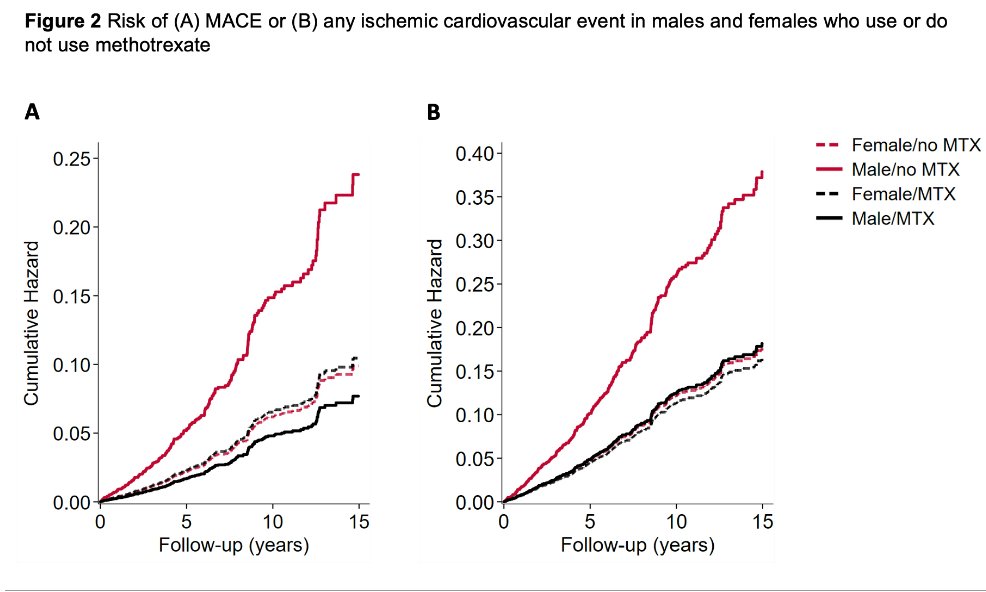
Karpouzas et al. MTX reduces IHD in males but not females with RA. 4362 patients. 66% lower risk MACE and 55% lower risk any ischaemic CVE. Abstr#1627 #ACR23 @RheumNow https://t.co/MC4W0dinUv https://t.co/1hkBoawt4b
Richard Conway ( View Tweet)
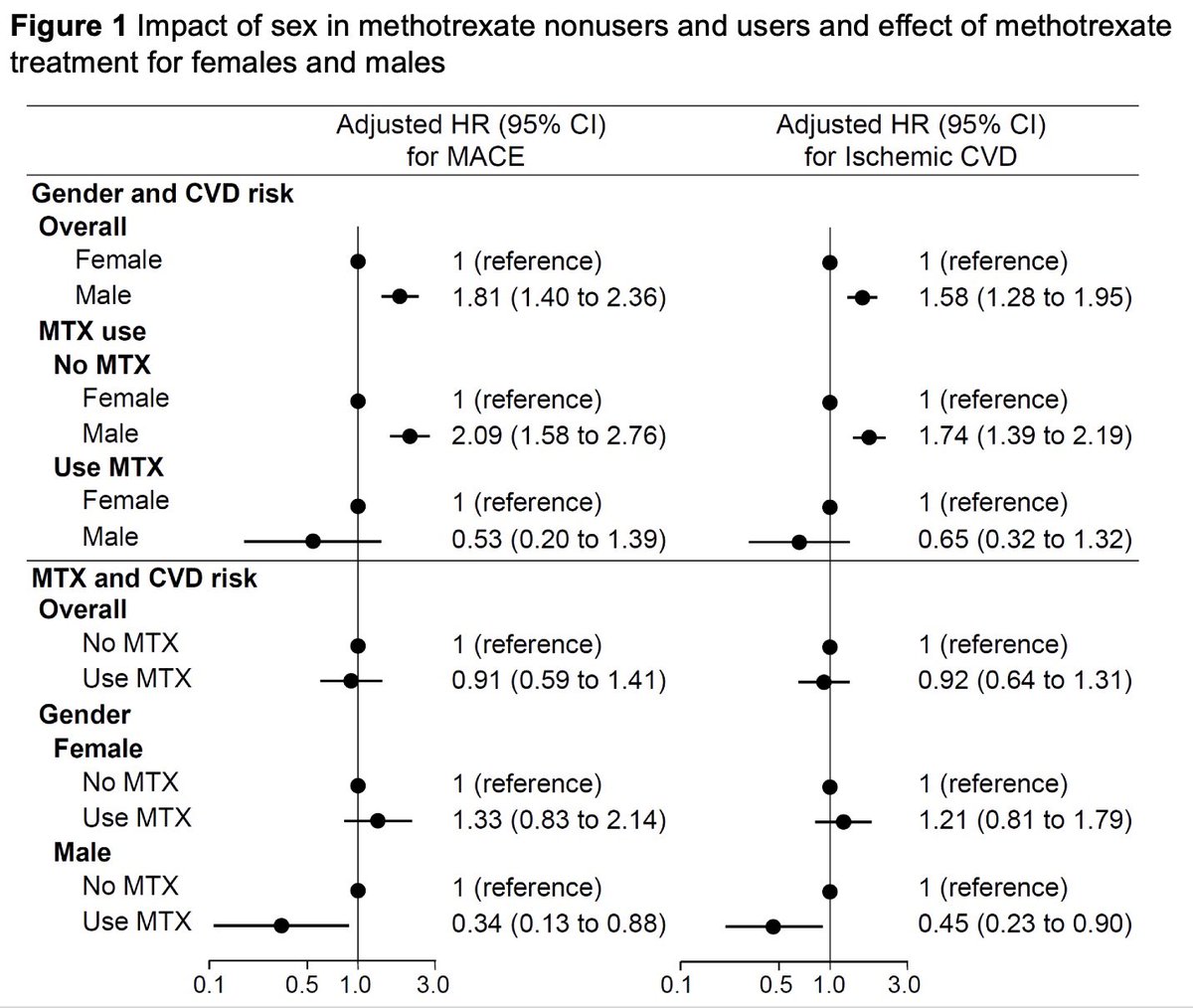
RA males 81% increase MACE & 58% ischemic CVE
2 folds Males>Females in MTX non users
Makes MTX users reduction 66% & 55% risk MACE & ischemic CVE and no diff w/ females
MTX use not assoc w/ reduction MACE in females
@RheumNow #ACR23 ABST1627 https://t.co/qbAc2bWdcM
Aurelie Najm ( View Tweet)
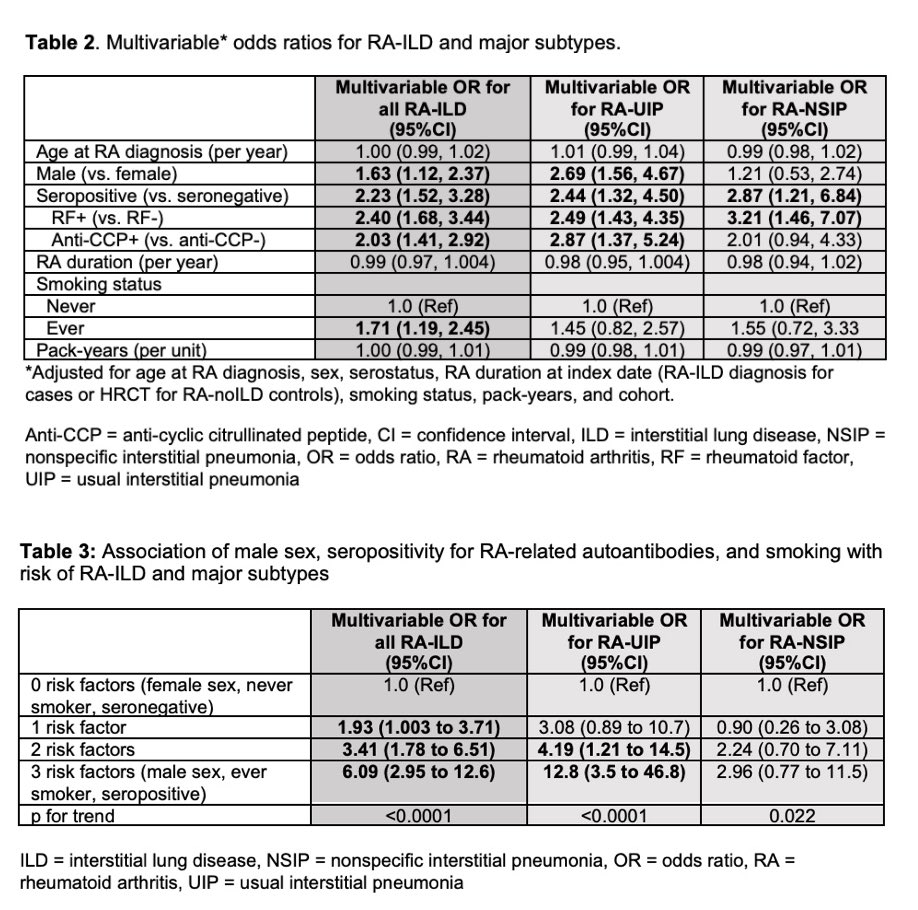
RA-ILD is an heterogeneous condition
Different risk factors identified dep/ on radiographic pattern
RA-UIP:
-male sex OR 2.7
-ACPA+ OR 2.2
-male + ACPA + smoking OR 13
RA-NSIP:
-RF+ OR 3.2
Likely to support different pathological mechanisms
@RheumNow #ACR23 ABST1269 https://t.co/rC2F9YAceQ
Aurelie Najm ( View Tweet)
Biologics are working for ankylosing spondylitis, even in reducing cardiovascular mortality!
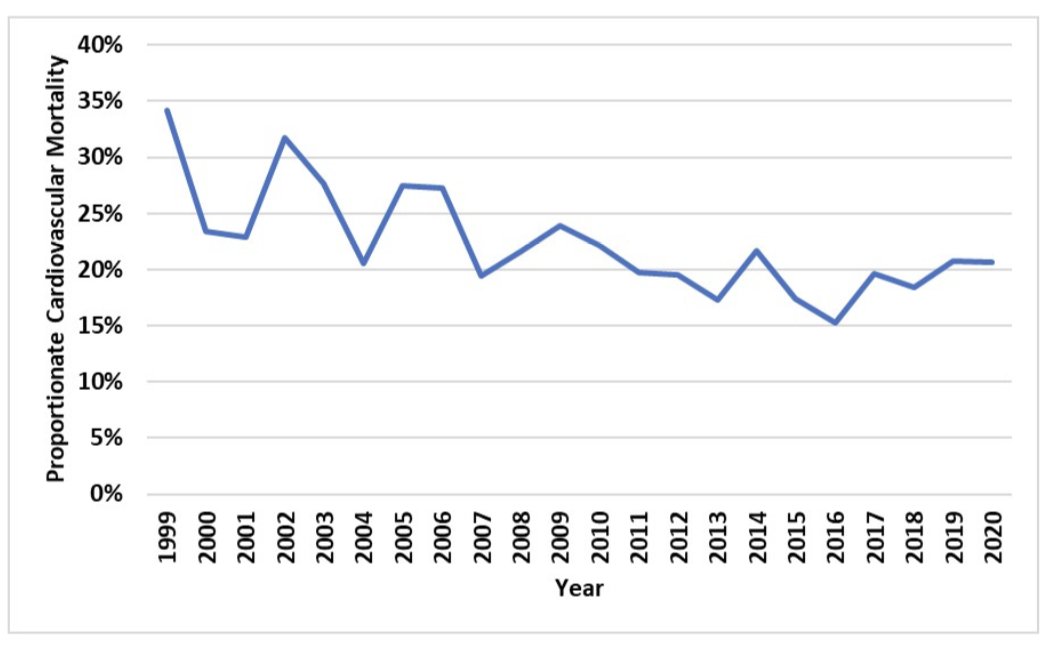
Large retrospective study of over 4k pts over 20 years showed decrease in CV mortality from 34% in 1999 to 21% in 2020
@RheumNow #ACR23 Abs#1399
#ACRbest https://t.co/wKCIXHza0v
Robert B Chao, MD ( View Tweet)

LV mass higher in pts with SLE nephritis.Nested case-control study 48 SLE pts +/- LN. LV mass higher w/LN (66.9 g/m2) vs pts w/o LN (54.8 g/m2, p=0.035). Higher LV mass may increase risk for CV events as CHF, arrhythmias and CV mortality. @RheumNow #ACR23 abst#1447
TheDaoIndex KDAO2011 ( View Tweet)
ABS0122 at #ACR23
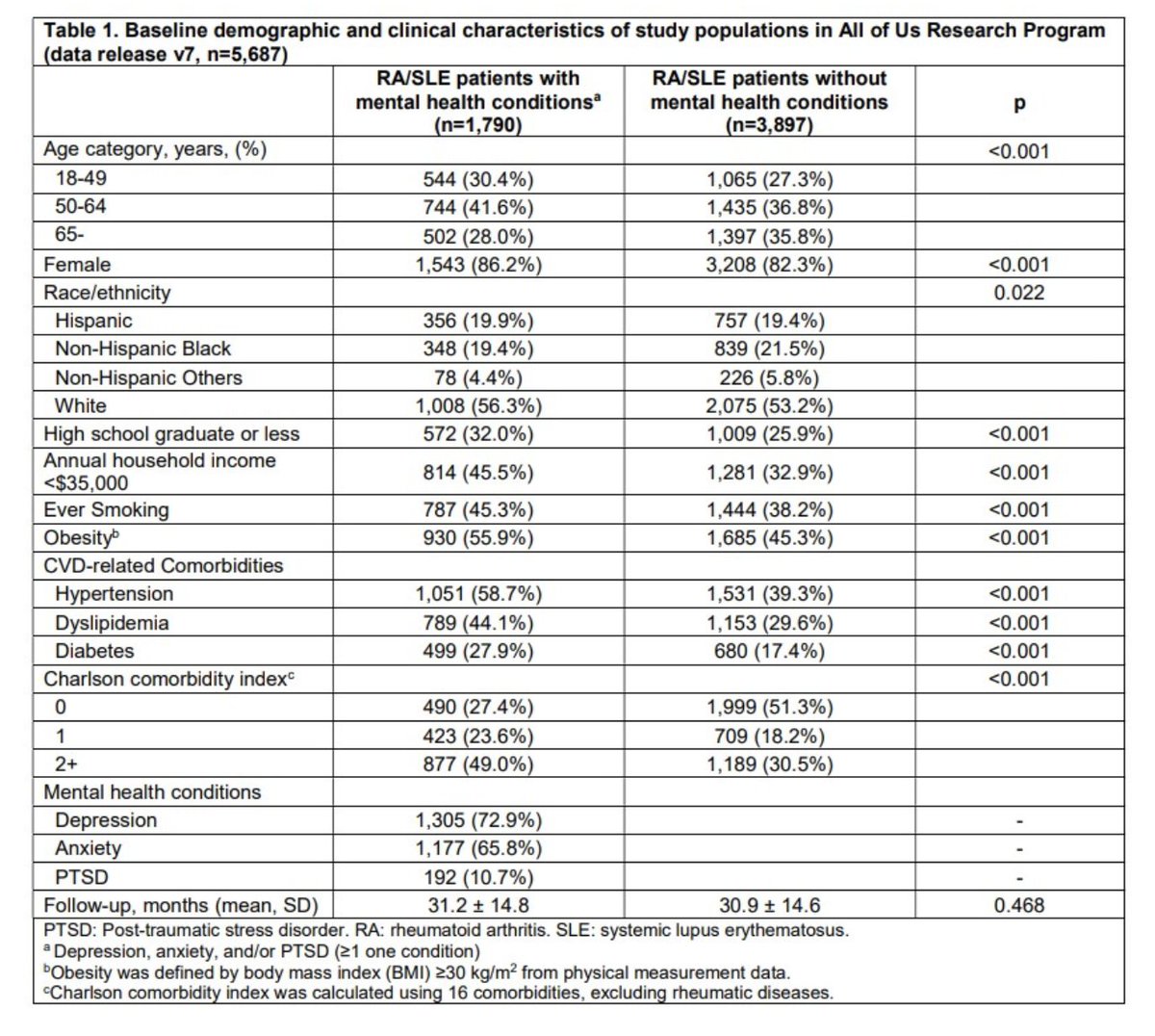
⭐️Risk of acute MI, stroke & death signif ⬆️ among RA/SLE pts w/ depress, anxiety, &/or PTSD vs w/o both RA/SLE
➡️U.S. pts: 3825 RA, 1862 SLE --> 1790 w/ above mental health dz, no prior CVD
➡️HR 1.28 after adjusting for🚬, obesity, & comorbidities
@RheumNow https://t.co/sXMFtaKmYB
Meral K. El Ramahi, MD MeralElRamahiMD ( View Tweet)

I vote for the ❤️
Several abstracts evaluated cardiovascular event prevalence and screening tools using ECHO, carotid ultrasound as current CV risk calculators are inadequate when assessing SLE CV risk. See my blog - just published @RheumNow
https://t.co/XLc0YHtJ0B https://t.co/oF0fXBRM6O
TheDaoIndex KDAO2011 ( View Tweet)
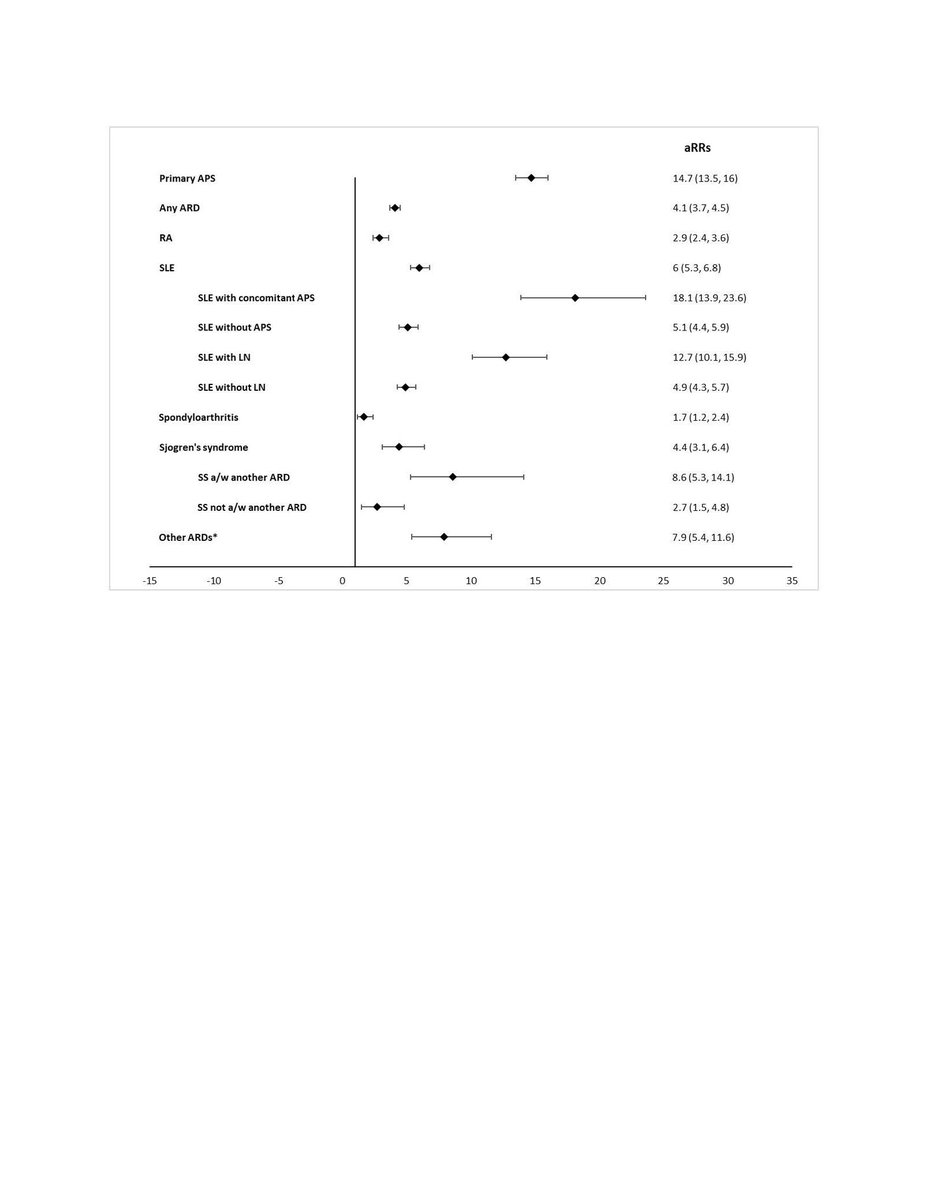
Pregnant women with ARDs esp. SLE nephritis and primary APS have significantly higher risks for acute CVEs compared to those without these conditions. 25-30% of CVEs occurred during the postpartum period, Dhital R Abst#0722 #ACR23 #ACRBest @RheumNow https://t.co/m9FjsAu64N https://t.co/1dyTzgH97A
Dr. Antoni Chan ( View Tweet)
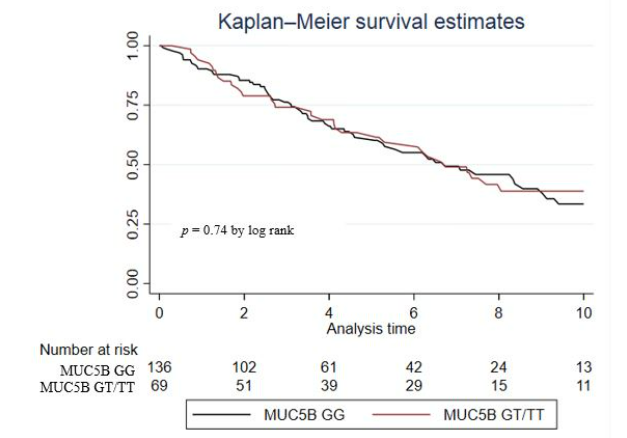
Klein et al. 205 RA-ILD. MUC5B not significantly associated survival, although wide CIs, aHR 0.75 (0.45, 1.24). Abstr#0772 #ACR23 @RheumNow https://t.co/ZfIIr2BbbR https://t.co/47DPYWNpL9
Richard Conway ( View Tweet)
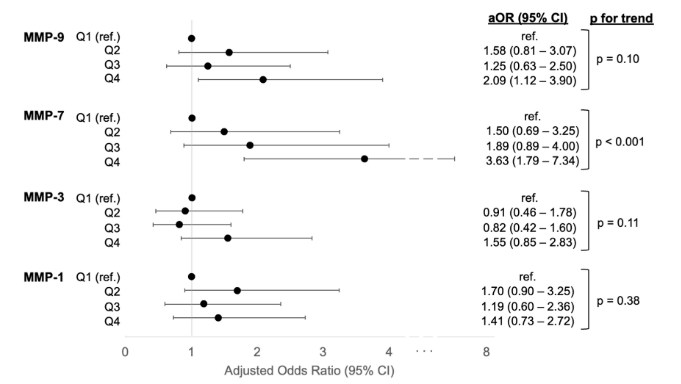
Plasma MMPs and RA-ILD. Strong association MMPs 7 & 9 with prevalent RA-ILD. Abstr#0770 #ACR23 @RheumNow https://t.co/5qWeK3lAly https://t.co/SyZY2OhcbH
Richard Conway ( View Tweet)
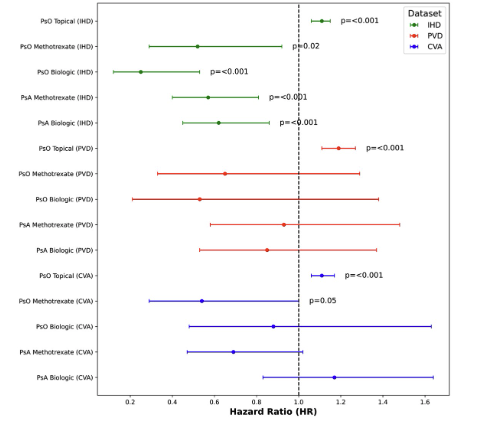
Ab#498 Does DMARD for PsO and PsA decrease MACE?
#ACR23 @RheumNow
Retrospective database Israeli study.
PsO, PsA on MTX or bDMARD: lower MACE compared to health matched controled (HR 0.45-0.68, p<0.001)
Pts on topical Rx had marginally Increased MACE (HR 1.14, p <0.001) https://t.co/0uRgjzYbFp
Eric Dein ( View Tweet)
Plenary 1 #ACR23
CVE in ARD/APS is a significant risk factor during pregnancies and the risk stays even after delivery for a significant amount of time. California based administrative data study! abst#722 @RheumNow https://t.co/HawhS4Gqko
Bella Mehta bella_mehta ( View Tweet)
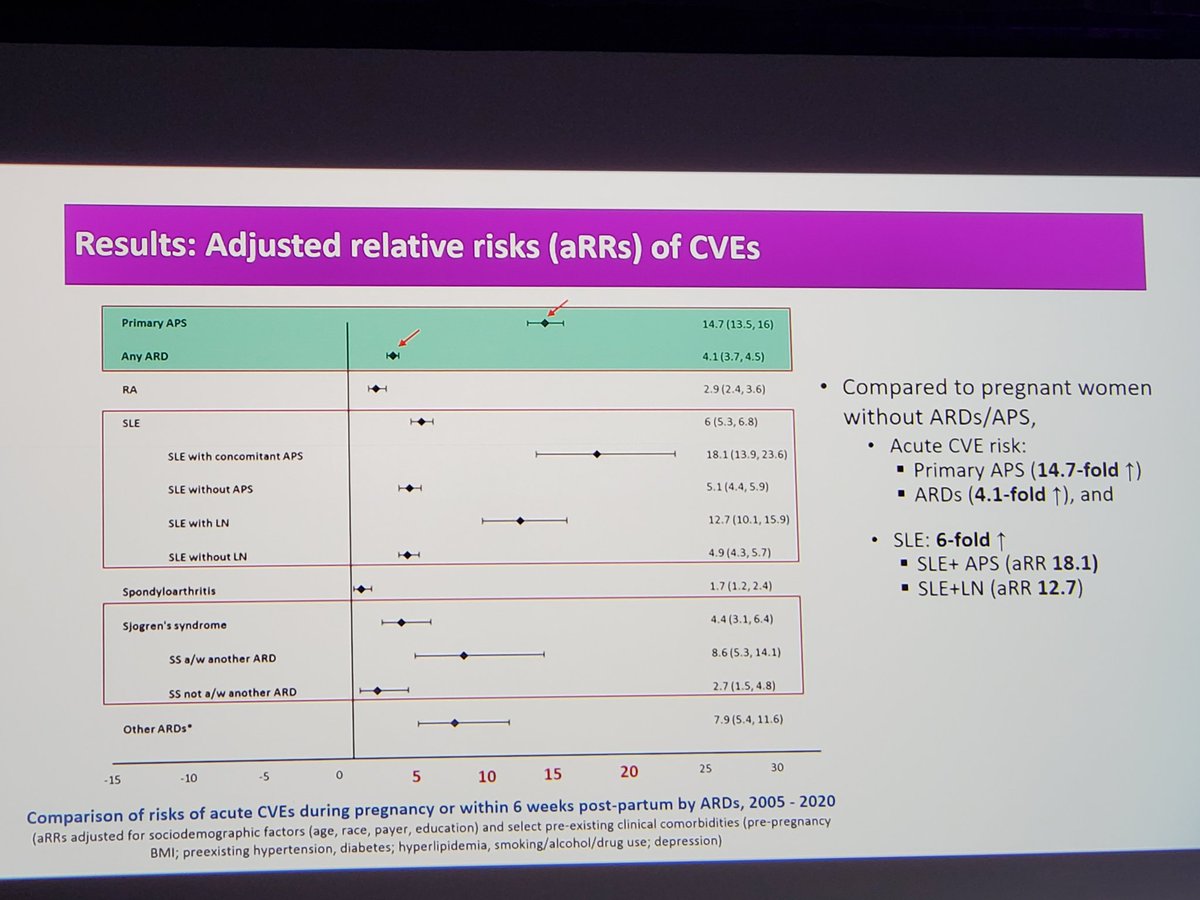
Plenary talk by Dhital etc al, shows increased risk of acute CV events in pregnant rheumatic, SLE, APS pts, esp if nephritis or APL+. #ACR23 Abstract 0722 https://t.co/pG0PqzVtIU
Dr. John Cush RheumNow ( View Tweet)
Non invasive screening for pulmonary involvement in early RA
Combination of PFT and Lung 🫁 US:
-50% with interstitial or focal changes or pleural effusion on US
-58% with abnormal DLCO
Correlation w/ higher disease activity.
Pathological meaning?
@RheumNow ABST 0393 #ACR23 https://t.co/BBcOEgcJK2
Aurelie Najm ( View Tweet)
Does knowing ischemic stroke subtypes among SLE patients matter?
This study by Hopia et al 👉54% of ischemic strokes in 56 SLE pts were APS/aPL & cardioembolic origin (accdg to TOAST) & +assoc with STAT4 gene.
#ACR23 ABST0579 @RheumNow https://t.co/Ut8QPpQNQp
sheila ( View Tweet)
#CV risk in #AxSpA in Korean population study N=71001, age 42, 71%M but 16% #MTX, 58% #SSZ. #TNFi vs none 30% less CVE. IL17 NO CV reduction but ?confounded by line of #Rx and v large N for TNFi. Study stated PRIOR to IL17i approval #ACR23 @ACRheum @RheumNow L11 poster ?Rx bias https://t.co/3Sft5KUlLa
Janet Pope ( View Tweet)





