Beyond malignancy, look out for LICATS with CAR-T Save
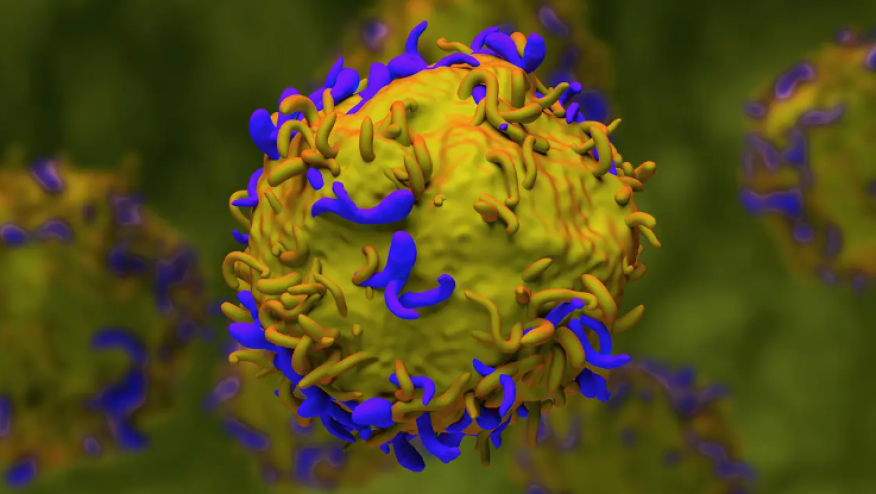
CD19 chimeric antigen receptor (CAR) T cell therapy took the centre stage in 2022 where data pertaining to a successful case series of 5 patients with refractory SLE were published by Prof Schett’s group. Since then, this area of therapeutic has expanded exponentially.
Our growing enthusiasm was slightly dampened though when the FDA required all six approved CAR T-cell therapies in oncology to include a black box warning regarding the risk of second primary malignancies in January 2024. Thus, we have become cautiously optimistic about the development of CAR-T and other CAR-based therapies in autoimmunity. Beyond malignancy, cytokine release syndrome and immune effector cell-associated neurotoxicity syndrome (ICAN), is there anything else that we should look out for from the perspective of safety in autoimmunity?
At ACR25 Convergence Conference in Chicago, Prof Schett’s group described a new form of toxicity in patients with autoimmune disease receiving CAR T-cell therapy, most likely due to the cleansing of immune cells from the affected organs.
Of 39 patients studied (i.e. SLE = 20; systemic sclerosis = 13; and idiopathic inflammatory myopathies = 6), 54 local reactions in 30 patients (77%) with a median time of onset of 10 days (IQR 9–21) from CAR T-cell infusion and a median duration of 11 days (5–14) were observed and recorded. These reactions were termed local immune effector cell-associated toxicity syndrome (LICATS) and occurred during the B-cell aplasia phase. LICATS appeared to involve organs previously affected by the respective autoimmune disease. The most frequently affected organs were the skin (35%) and the kidneys (22%). Most cases of LICATS were mild and only three cases were grade 3. Some patients needed to be treated with a short course of glucocorticoid. Fortunately, all cases of LICATS resolved without sequelae (Abstr# 1537).
During the poster presentation session, the researchers also reported that the skin biopsy did not reveal abnormal pathology (i.e. active cutaneous lupus). This finding is interesting and in contrast to the finding from my group. We previously published that following therapy with rituximab, flares of subacute cutaneous lupus or chronic cutaneous lupus occurred in some patients who either had no skin disease or had acute cutaneous lupus at baseline (i.e. a switch in subtype). Accordingly, post-treatment biopsies confirmed typical active SLE histology in lesions which might indicate a change in immune regulation following B cell-targeted therapy (PMID: 25707733).
Whatever the pathology is here, the study presented at ACR25 above is useful and reminded us to be aware of potential side effects from CAR-T therapies and other deep B-cell depleting agents as safety of our patients is paramount.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.