Health inequities in rheumatology: A central theme Save

This year at EULAR, health inequalities have taken centre stage as fundamental drivers of outcomes in rheumatic and musculoskeletal diseases (RMDs). Across multiple sessions and studies, delegates are presenting compelling evidence and ground-breaking research demonstrating that who you are, where you live, and what resources you can access truly do shape the trajectory of chronic illness just as much as biological factors.
Data from the EULAR RheumaFacts initiative has revealed the extent of inequities across Europe in access to rheumatology care (Abstract OP0025). Among 31 EULAR member countries, the availability of rheumatologists varied dramatically, from fewer than one per 100,000 inhabitants in some regions (0.6 in Ukraine) to more than eight in others (Hungary). Access to reimbursed physiotherapy, psychological care, and advanced treatments such as biologics and targeted synthetic DMARDs (b/tsDMARDs) was similarly inconsistent. In nearly half of the participating countries, patients lacked routine access to either physiotherapy or mental health support, two key aspects of holistic RMD care. This disparity persists despite a shared burden of disease and a common aim of preventing long-term disability.
Importantly, these system-level inequities are compounded by patient-level social determinants. A study using data from the National Early Inflammatory Arthritis Audit (NEIAA) by our group found that low health literacy, particularly difficulties finding or understanding health information, was associated with more active disease, higher work productivity loss and poorer mental health outcomes (Abstract OP0026). Even in a publicly funded health system, the ability to engage with and navigate care remains uneven. It is a sobering reminder that health equity is not achieved by access alone, but by ensuring that access is meaningful, relevant, culturally-sensitive and usable to all patients.
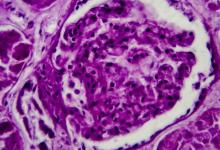
The impact of health inequities in people with systemic lupus erythematosus (SLE) is increasingly recognised. The importance of social context has been reinforced by Swedish registry data showing that people with SLE with a lower income or education levels experience significantly greater risks of organ damage and mortality (Abstract OP0200). The findings are particularly striking because, again, they emerge from a country with universal healthcare coverage, underscoring that equity in access does not automatically translate to equity in outcomes. Factors such as sick leave, receipt of disability benefits and educational attainment shaped the likelihood of long-term complications and death, even when healthcare costs were not the primary barrier.
Together, these studies paint a bleak picture. Health inequalities in RMDs are not confined to under-resourced regions or to marginalised populations. They manifest across the countries, from challenges in both universal and private health systems, to personal challenges navigating care within those systems. They affect outcomes that matter, such as pain, disability, disease control and life expectancy.
The emerging data calls for more than simply acknowledgment of health inequities. Targeted interventions to improve health literacy, better workforce distribution, equitable reimbursement policies, and support structures for socially vulnerable patients are not optional. They are essential to improving outcomes across the RMDs
Research such as those described above, and the many other abstracts and sessions on social determinants, bring with them a sense of urgency. Events such as EULAR provide an opportunity to reimagine what equitable, patient-centred rheumatology care can look like, and facilitate important discussions and initiatives to ensure inequalities continue to be recognised as key drivers of disease.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.