What you need to know about scleroderma-related lung fibrosis Save
What do you need to know about scleroderma-related lung fibrosis as a practicing rheumatologist?
Systemic sclerosis or scleroderma related lung fibrosis (also known as interstitial lung disease or pulmonary fibrosis) is seen in 50-70% of patients, depending on the modality utilized to diagnose it. ILD is leading cause of death in SSc, including in those with sine/ limited cutaneous SSc. Recent guidelines from the ACR/ Chest and ERS/ EULAR have published guidelines on the screening, diagnosis and management of SSc-ILD. Here are takeaways from these guidelines and my practice.
- ILD is common in SSc and gold standard to diagnose early ILD is the HRCT of chest. Chest x-ray, physical examination (including auscultation) and PFTs are complementary to HRCT but can miss early ILD.
- Although 50-70% have ILD on HRCT, 25-35% meet the criteria progressive pulmonary fibrosis.
- I recommend that every new patient with early SSc (within first 7 years of onset of SSc) should get PFT and HRCT of chest.
- If the HRCT is negative, the recent guidelines differ in these recommendations. The ACR/ Chest guidelines recommend close follow up and repeat HRCT of chest in patients with high-risk features, and the ERS/ EULAR guidelines recommend annual HRCT. With low dose HRCTs available, this may be an option in those who have high risk features.
- If a patient has ILD, they should get FVC with DLCO, preferably in the same institution, every 3-6 months and ambulatory oxygen evaluation till stabilization is documented. After that, we PFTs and ambulatory oxygen indefinitely on annual basis.
- These patients should be managed in a multidisciplinary setting with pulmonologist and radiologist.
- Patients should be educated about ILD and relationship to gastroesophageal reflux diseases, and appropriate vaccinations should be recommended (I recommend annual influenza, annual Covid-19, Prevnar-20, Respiratory Syncytial Virus, and Shingrix vaccines).
- Not every patient with SSc-ILD requires treatment. In my practice, due to universal HRCT, some patients have minimal ILD, normal PFTs and no ILD specific symptoms (we have termed it as subclinical ILD). These patients can have a close follow up, unless they have risk factors, esp. early disease, progressive worsening of skin, elevated acute phase reactants, and positive anti-topoisomerase Ab. In our practice, ~ 30% meet the subclinical definition and approximately 15% are treated with available therapies.
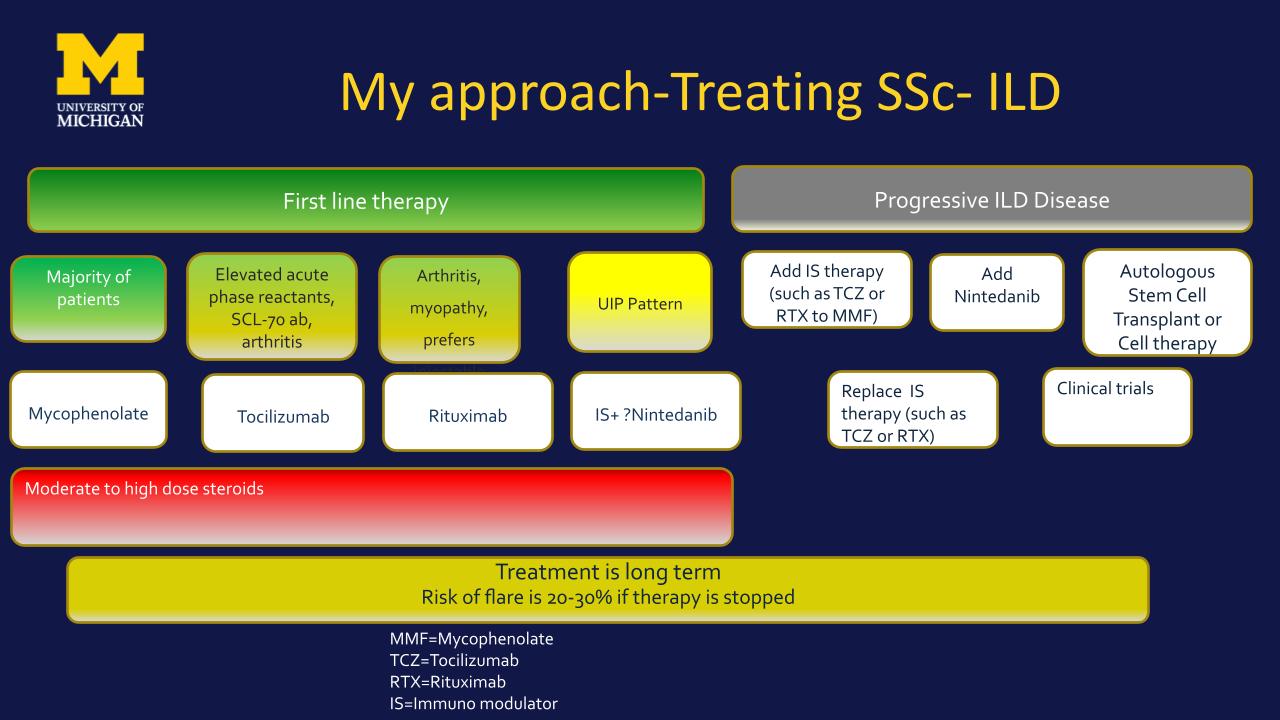
- Both the ACR/ Chest and ERS/ EULAR guidelines recommend immunosuppressive therapies with mycophenolate mofetil as the first agent.
- ACR/ Chest and ESR/ EULAR recommend tocilizumab for those with progressive skin disease and elevated acute phase reactants.
- Both recommend first line nintedanib with at least moderate fibrosis on HRCT and/or UIP pattern on HRCT and no extra pulmonary signs/ symptoms.
- SSc-ILD is slow progressive disease, and clinicians need to carefully assess for progressive disease. In my practice, it is a combination of longitudinal trends in FVC and DLCO, increased or new symptoms, and progression on HRCT. This requires every 3-6 months PFTs, assessment of shortness of breath and cough at each visit, and annual HRCT, especially in early disease.
- Management for progressive fibrosis varies and is determined by available therapies.
- Clinical trials remain an important aspect for management of SSc-ILD.
- We have recently launched the first platform trial, called CONQUEST that is recruiting 400+ pts with early SSc with ILD and testing 2 novel therapies, nerandomilast (a PDE4b inhibitor) and amlitelimab (anti-OX-40L). https://srfcure.org/research/conquest/
- Finally, there is encouraging data on use of cell therapy for management of SSc, including SSc-ILD. More data is needed to assess the risks/ benefits of these therapies.
- Below are my current management strategies for SSc-ILD










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.