Articles By Md Yuzaiful Md Yusof, MRCP(UK), PhD

Impact of regulatory warning on JAK inhibitors
The development of JAK inhibitors represents an advance for the treatment of inflammatory rheumatic diseases. However, the enthusiasm in using this target has waned since the publication of the ORAL surveillance clinical trial in 2022. Subsequently, both the FDA and EMA issued a warning on using JAKi in patients with certain risk factors, e.g., ≥65 years, at increased risk of MACE, current smoker or past smoker and at increased risk of cancer, should other alternative treatment be available. So, how has this warning impacted on JAKi development and use?
Read Article
SLE Preview: abolishing refractory with CAR-T and better B-cell therapies
Inhibition of B cell activating factor (BAFF) and B cell depletion are the two most evaluated strategies over the last 15 years in the field of SLE therapeutics, with licensing of belimumab and off-label use of rituximab.
Read Article
ICYMI: Glucocorticoids-free zone in SLE?
For over 70 years, glucocorticoids, (GC) have been a part of standard therapy in SLE. They are classically used to not only induce remission or treat an acute flare, but also as maintenance therapy. They are a valuable 'friend' if used wisely, and can become a 'foe' if used excessively.
Read Article
Next generation JAK-inhibition strategies
It has been just over a decade since the approval of tofacitinib (JAK1/JAK3-inhibitor) by the US FDA for the treatment of rheumatoid arthritis. Since then, baricitinib (JAK1/JAK2-i), filgotinib and upadacitinib (both selectively targeting JAK1) also have been licensed for the treatment of rheumatoid arthritis. As there are many more JAK-inhibitors evaluated in clinical trials currently, how do you stand out?
Read Article
Early aggressive treatment in SLE: are we there yet?
Early treatment with DMARDs has revolutionised the outcomes of patients with rheumatic arthritis. However, this concept has not been fully extrapolated to other autoimmune rheumatic diseases such as systemic lupus erythematosus.
Read Article
The impact of SGLT2-inhibitor on SLE outcomes
Since chronic kidney disease is one of the strongest CV risk factors, any new strategy to reduce proteinuria and avoid a decline in renal function may likely improve patient outcomes. In large cardiovascular outcome trials, the use of a fairly new-kid-on-the-block therapy, sodium–glucose cotransporter-2 inhibitors (SGLT2i) appear to be both cardio and renal-protective. Would the use of SGLT2i have the same impact in SLE?
Read Article
Glucocorticoids-free zone in SLE?
For over 70 years, glucocorticoids, (GC) have been a part of standard therapy in SLE. They are classically used to not only induce remission or treat an acute flare, but also as maintenance therapy. They are a valuable 'friend' if used wisely, and can become a 'foe' if used excessively.
Read Article
A step change towards self-empowerment for people living with SLE
In my focus group consisting of people living with SLE and their carers, one of the keys issues raised by them was pertaining to poor reliable information about their condition. At the 2023 EULAR Congress in Milan, I learned about the wide scale dissemination and international launch of Lupus100.org project.
Read Article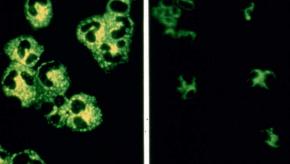
ANCA-associated vasculitis: beyond therapy with rituximab?
Following the success of Phase 3 randomised controlled trials of non-renal and renal vasculitis, therapy with rituximab has tremendously improved the outcomes of AAV patients. However, some patients are unable to taper their glucocorticoids during rituximab therapy while others appear to be refractory to therapy, particularly those with EGPA. Hence, what are other current or future approaches beyond rituximab?
Read Article
Targeted therapies in Sjogren’s syndrome: are we close?
There is a clear unmet need for new and effective therapies in primary Sjogren’s Syndrome (pSS) patients, as there are no current licensed therapies.
Read Article



