ANCA-associated vasculitis: beyond therapy with rituximab? Save
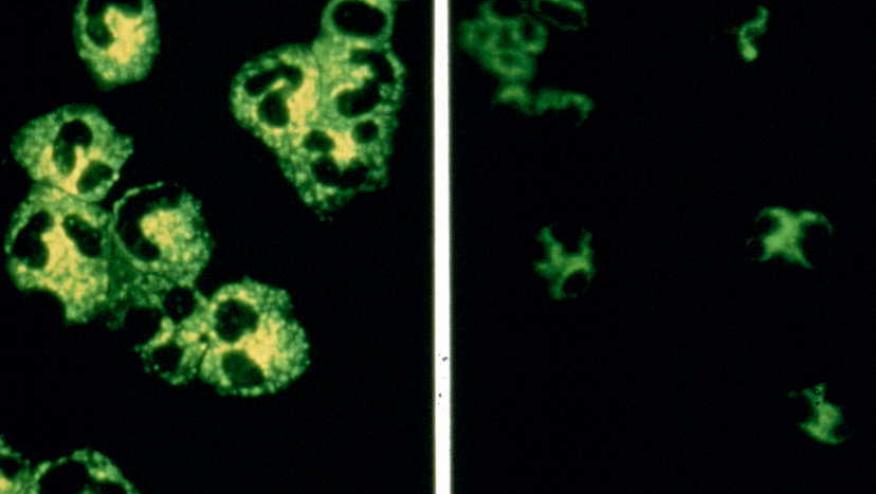
AAV is a group of multi-system autoimmune small vessel vasculitides which includes granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA).
Following the success of Phase 3 randomised controlled trials (RCTs) of non-renal (RAVE) and renal vasculitis (RITUXVAS), which showed no inferiority of rituximab over cyclophosphamide for remission induction of AAV, therapy with rituximab has tremendously improved the outcomes of AAV patients. However, some patients are unable to taper their glucocorticoids during rituximab therapy while others appear to be refractory to therapy, particularly those with EGPA. Hence, what are other current or future approaches beyond rituximab?
Avacopan, a C5a receptor inhibitor was approved by FDA and EMA in 2021. In the ADVOCATE Phase 3 RCT, avacopan when used as add on to either cyclophosphamide or rituximab was non-inferior to prednisolone taper with respect to remission at Week 26 but was superior to prednisolone taper in sustained remission at week 52 and with lower glucocorticoid toxicity index. Since up to 2/3 of patients may experience a relapse following remission induction with cyclophosphamide and would require a switch of therapy to rituximab, current approach favours remission induction with rituximab as first line agent. At the 2023 EULAR Congress in Milan, the investigators performed sub-group analyses of the ADVOCATE trial which included patients who received remission induction with rituximab only (i.e. 65% of total patients). The results showed similar and favourable efficacy (sustained remission, relapse rate, eGFR, albuminuria, and less GC toxicity) and safety profile of RTX + avacopan over RTX + prednisolone taper, consistent with data from the main ADVOCATE trial (POS0222).
Rituximab is licensed for remission induction of GPA and MPA. A phase 3 RCT in EGPA in France showed no superiority of rituximab over conventional therapeutic therapy pertaining to remission induction of vasculitis. Nevertheless, rituximab therapy appeared to be effective in some EGPA patients particularly those with ANCA-positivity based on cohort studies. The first and only therapy approved by FDA and EMA in EGPA is mepolizumab, an IL-5 inhibitor. Is any other promising therapy in the pipeline for EGPA?
At the 2023 EULAR Congress, Dr Bettiol (OP0304) presented data on the effectiveness of benralizumab, an IL-5 receptor inhibitor using European multicentre cohort study of 121 patients. It is important to note that benralizumab was given to EGPA patients for eosinophilic asthma indication for which this therapy is licensed. In terms of eosinophilic asthma, the proportion of patients reporting active symptoms decreased from 94% at baseline to 36% at 6 months. While for EGPA, the proportion of patients meeting the criteria for complete response (defined as BVAS=0 and prednisolone ≤4mg/day was 16% at 3 months, 26% at 6 months and 46% at 12 months. Active ENT manifestations improved from 70% at baseline to 46% at 6 months. This real-world study suggests that benralizumab could be effective in treating both respiratory and overall EGPA disease activity. A Phase 3 RCT of benralizumab in EGPA is ongoing and the results will be eagerly awaited.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.