All News
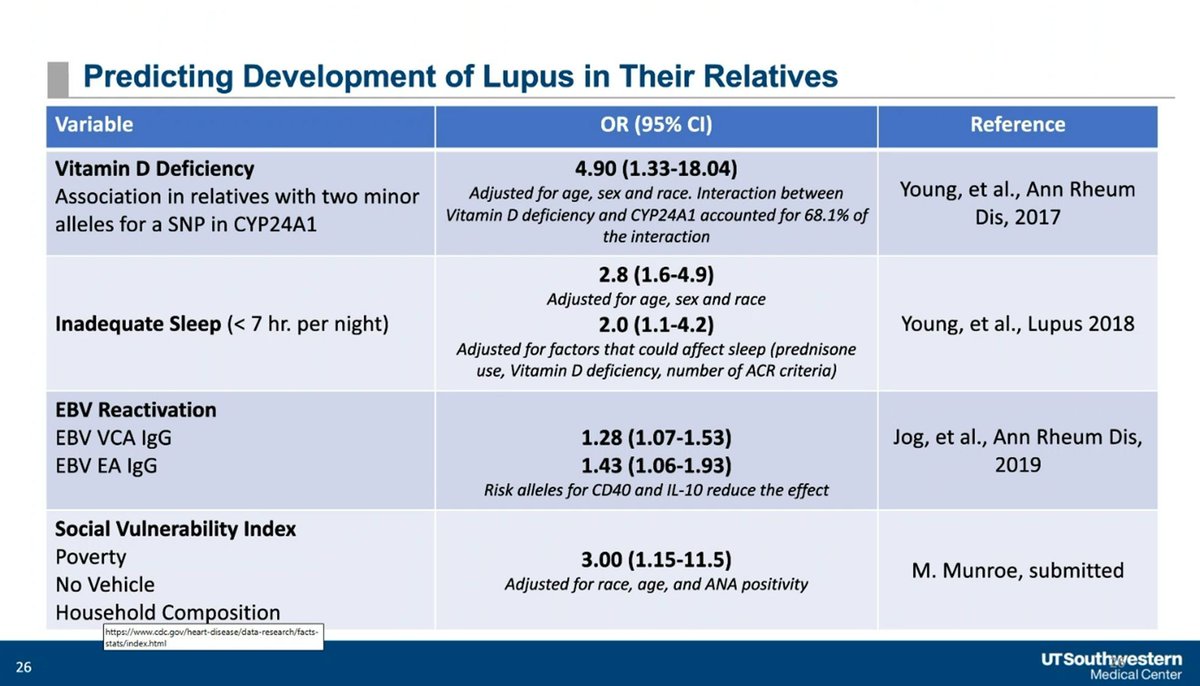
Early vs Delayed Belimumab in Lupus
An economic evaluation of early vs delayed use of the Blys inhibitor, belimumab (BEL), in systemic lupus erythematosus (SLE) has shown both cost effectiveness and clinical utility of early BEL initiation in active lupus patients.
Read ArticleReferral Rules to Live By (2.20.2026)
Dr. Jack Cush reviews the news and journal reports from this past week on RheumNow.com. Highlights include referral rules, combination biiologics in psoriasis and don't use JAK inhibitors in pregnancy.
Read ArticleReferrals - Orthopedics or Rheumatology?
“Orthopedics or rheumatology, who should I see?" A question, often asked with urgency, posed by those who genuinely don’t know who to see for a musculoskeletal (MSK) complaint. Inquiring patients, family, or other physicians may be one forum for such a request. Another occurs in the hospital and clinic when referrals for MSK issues can go in either direction. How would you guide such requests? And what would your answers be based on?
Read ArticleMaui Potpourri (2.13.2026)
Dr. Jack Cush reviews the hot item takeaways from last week's RheumNow.Live 2026.
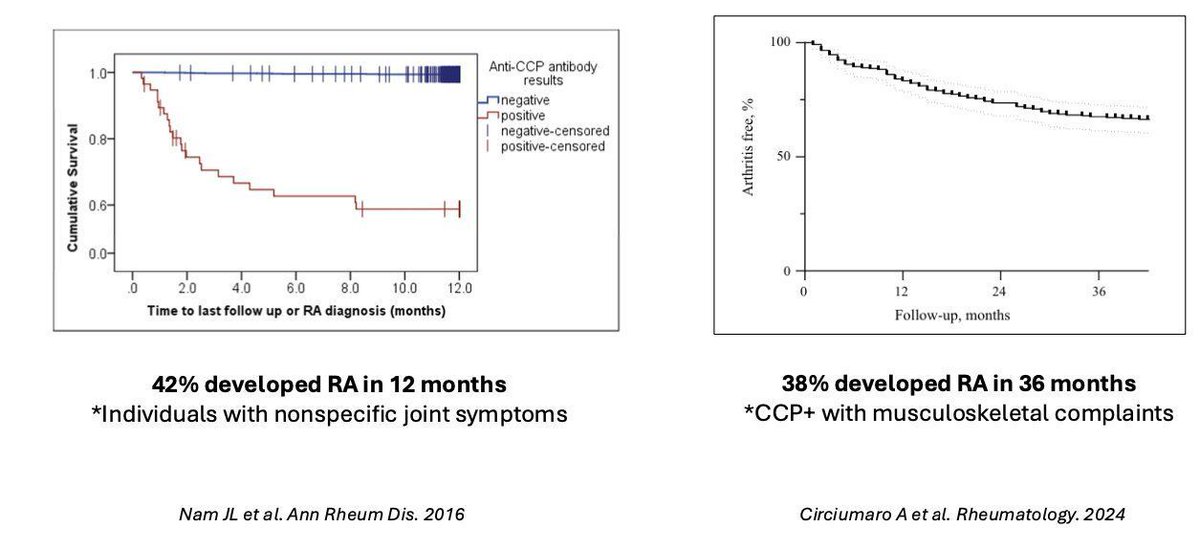
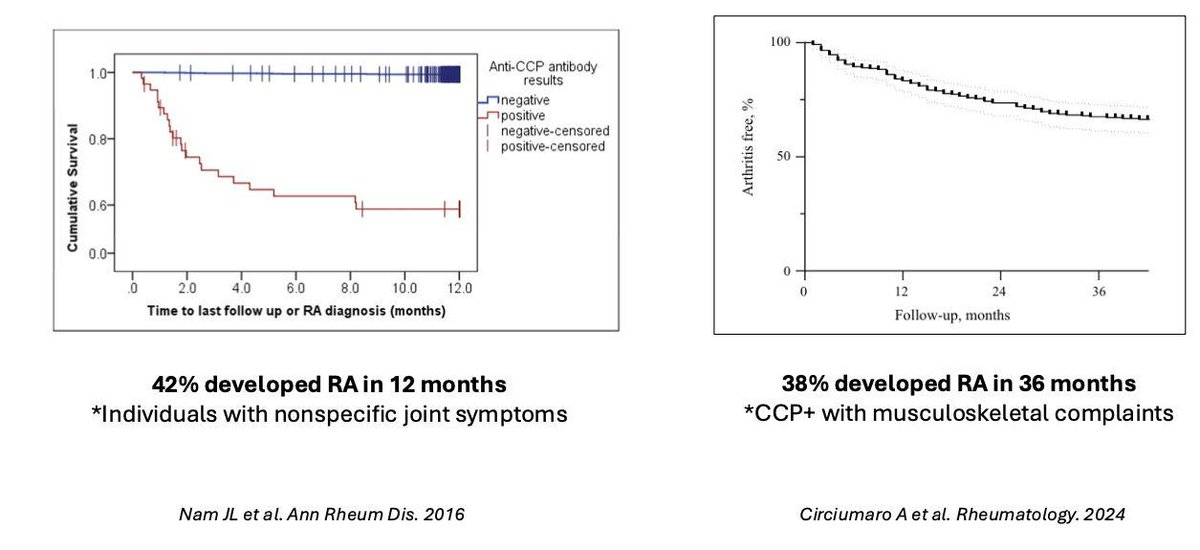
Read ArticleALTO: Long-Term Abatacept Outcomes in At-Risk RA
Lancet Rheumatology has published the ALTO results - long term outcomes of the APIPPRA trial, demonstrating that treatment with abatacept (ABA) in at risk patients can delay progression to rheumatoid arthritis (RA) for up to 4 years.
Read ArticleGiant Cell Arteritis Outcomes in Canada
A retrospective cohort study of patients with giant cell arteritis (GCA) demonstrates relapses are common and seen in nearly half of patients, were common after treatment is stopped and is not effectively averted by methotrexate (MTX).
Read Article