All News
Emergency Department Visits by Rheumatoid Patients
A Canadian population study shows that rheumatoid arthritis (RA) patients have 30% higher emergency department (ED) visit rates for Ambulatory Care Sensitive Conditions (ACSCs) compared to age- and sex-matched population controls.
Smartphones and Rheumatoid Flares
FORWARD Databank of Rheumatoid arthritis (RA) patients reveals that smartphone data can predict flares using PROs.
Nurse Practitioner Independence
A JAMA Viewpoint article reports on a March 2025 Nurse Practitioner (NP) Entrepreneurship Summit in Boston in March 2025 identifying barriers and opportunities to NP-owned medical practices.
Read Article
Links:
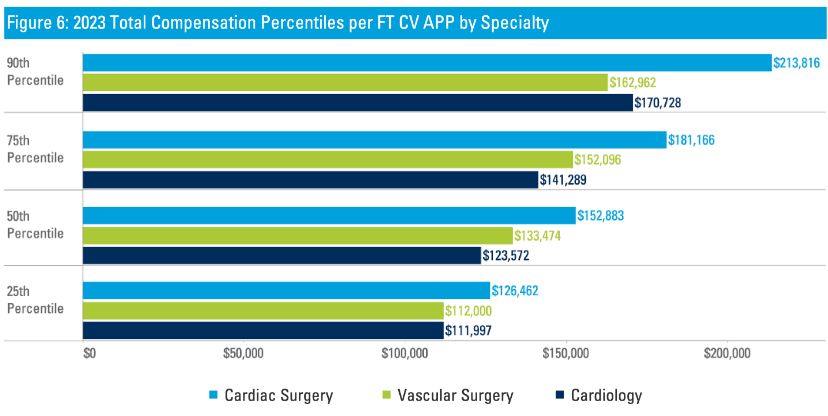
2024 Cardiology Income Survey - CV APP salary has incr 15% from 2019 -23, median=$123K - 50% of APP programs lead by an APP >90% work in outpt. clinics - 2/3 of prgs deploy APPs lipid & prevention management - 2 APPs for every 3 cardiologists https://t.co/gtdm5qN1qD https://t.co/cx2JUcw4U3
Links:


Dr. John Cush RheumNow ( View Tweet)


Links:



Links:






