All News
ACR21 Best Abstracts - Day 2
The RheumNow faculty reporters have been scouring and reporting on the best abstracts from the ACR. Here is a sampling of their choice abstract presentations reported during ACR 2020 Day 2 (#ACRbest).
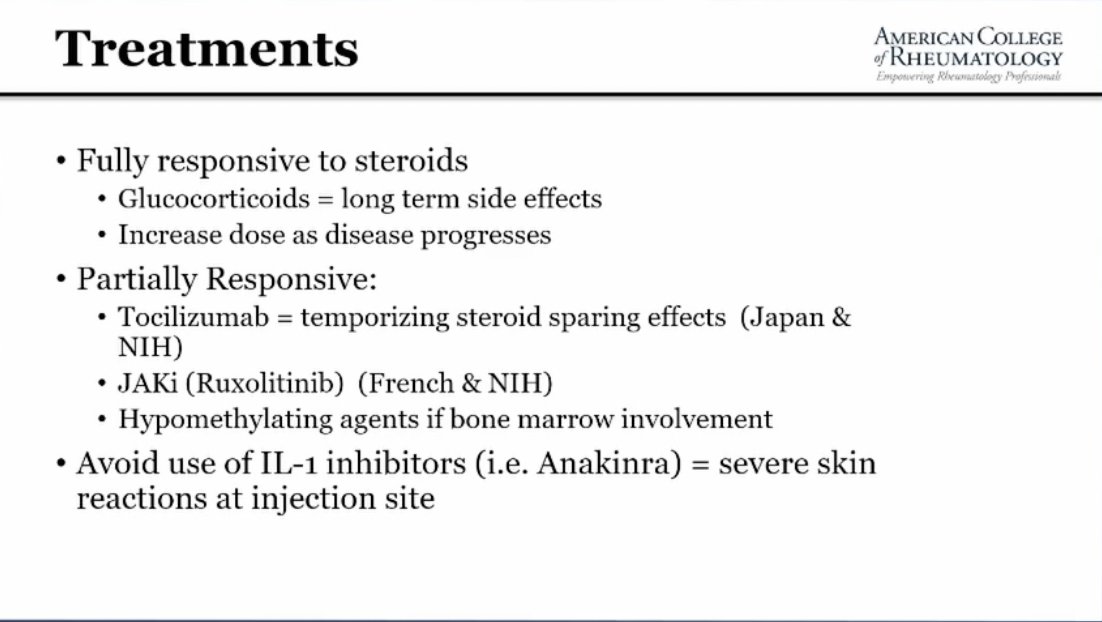
Read ArticleNovel treatment options for Giant Cell Arteritis
Giant cell arteritis is associated with significant treatment related morbidity due to the dependence on glucocorticoids as a treatment option. After sixty years of therapeutic stagnation, these are exciting times in the management of GCA. At this year's ACR Convergence meeting, encouraging data will be presented on options for GCA.
Read ArticleRheumNow Podcast – ACR Convergence Begins (11.5.2021)
Dr. Cush reviews the news, and kicks off ACR21 learning and how to take in the annual meeting.
Read ArticleBlacks with Systemic Sclerosis May Have More Severe Disease
New research presented this week at ACR Convergence, the American College of Rheumatology’s annual meeting, shows that Black people living with systemic sclerosis may have more severe disease and worse prognosis than patients in other racial or ethnic groups, and these worrying disparities may be driven by several socioeconomic factors (Abstract #1854). This poster will be presented Tuesday morning, November 9, 2021 in the Clinical Poster III (1836–1861) section on Systemic Sclerosis & Related Disorders.
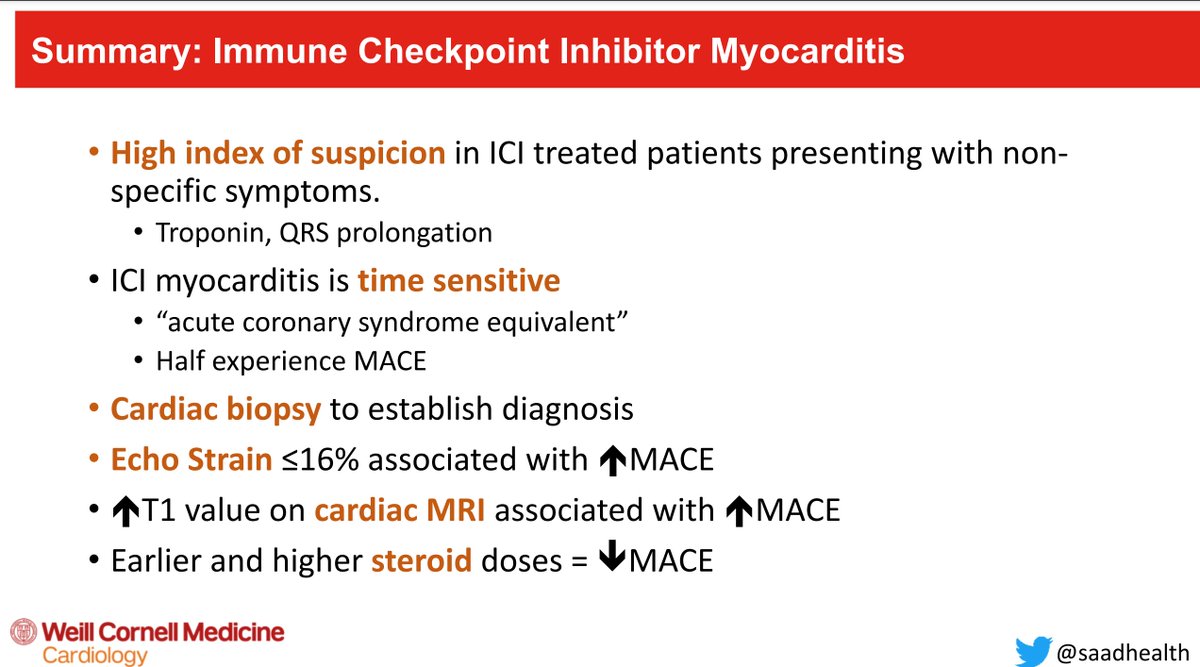
Read ArticleManagement of Immune-Related Adverse Events - ASCO Guideline
The American Society of Clinical Oncology, Inc (ASCO) has updated its guidelines and recommendations for the management of immune-related adverse events (irAEs) in patients treated with immune checkpoint inhibitor (ICPi) therapy. Below are select statements from this guideline.
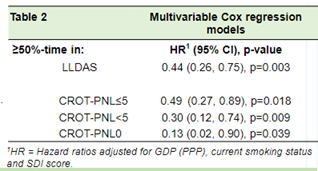
Read ArticleNOBILITY: a Trial of Obinutuzumab in Proliferative Lupus Nephritis
B-cell depletion therapy with obinutuzumab, a type II anti-CD20 monoclonal antibody, in lupus nephritis patients was shown to be effective in in combination with standard lupus therapies.
Read Article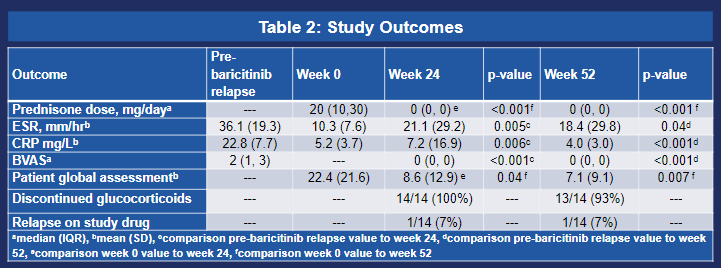

Janet Pope Janetbirdope ( View Tweet)

David Liew drdavidliew ( View Tweet)

Richard Conway RichardPAConway ( View Tweet)

Links:
Dr. John Cush RheumNow ( View Tweet)

Links:
Dr. John Cush RheumNow ( View Tweet)

Links:
Dr. John Cush RheumNow ( View Tweet)

Links: