2025 update of EULAR recommendations on lupus nephritis Save
At the 2025 EULAR congress in Barcelona, Prof Dimitrios Boumpas presented a summary of the updated EULAR recommendations on the management of lupus nephritis (LN). The most significant change in the treatment paradigm of LN is that the historic standard of care (SOC) (i.e. mycophenolate with glucocorticoids, GC) is now known to be inferior to several licensed combinations, as well as other unlicensed combination therapies.
Since the last EULAR recommendations in 2019, three targeted therapies, voclosporin, belimumab and obinutuzumab (when added to SOC) met their primary endpoints in Phase 3 RCTs. So, here are a few take home messages and my take on them.
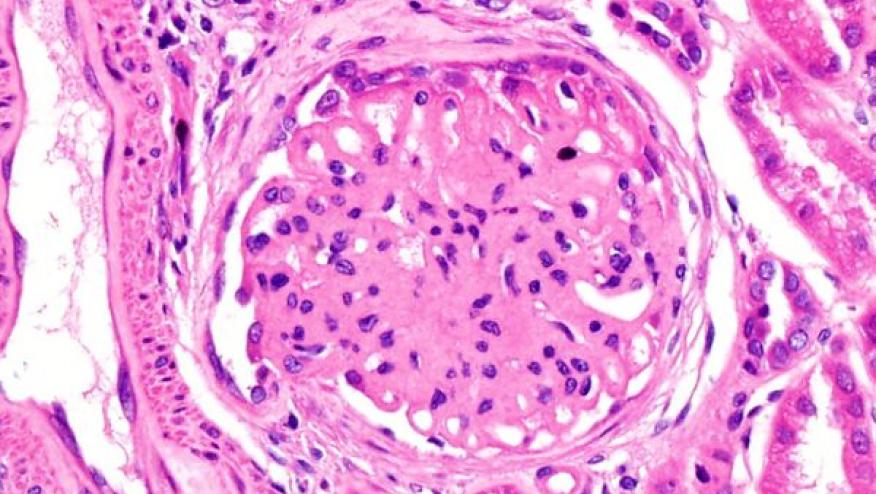
First: kidney biopsy is vital for assessment of suspected LN. Not only for diagnosis but also prognostication and to help tailor therapies. It also has a role to re-assess patients who are refractory to therapies.
Second: as per the 2025 ACR guidelines of LN, EULAR also recommend early use of quadruple therapies (GC + hydroxychloroquine + immunosuppressant [MMF or low dose Cyclophosphamide] + calcineurin inhibitor or Biologics [belimumab or obinutuzumab). The only difference is that the latter include obinutuzumab. The trial results were published after ACR guideline literature search. My reservation is that in the same statement, EULAR states that alternative regimens could include single-agent therapy with either MMF or low dose cyclophosphamide. I found this counterintuitive. Although I get that not all patients could tolerate quadruple regimens, efforts should be made to institute combination therapies as these regimens had the highest evidence. So, I would prefer the single-agent statement to not be included in the same line as the combination therapies.
Third: EULAR did not distinguish the choice of CNI or Biologics based on renal histology class. The REGENCY (obinutuzumab) trial excluded patients with Pure Class V only. In BLISS-LN (belimumab RCT) isolated class V LN made up 16% of the study patients. Lastly, in AURORA (voclosporin), about 14% patients had Pure Class V LN. The ACR and KDIGO guidelines pointed out a subgroup of patients who might be more suitable for belimumab (concurrent extra-renal activity and repeated flares), while for voclosporin, those with nephrotic range proteinuria.
Fourth: following IV methylprednisolone pulses for remission induction, EULAR allows for more generous oral GC (0.3-0.7mg/kg/day) compared to ACR (≤0.5mg/kg/day). But both advise to taper GC to ≤5mg/day by 4-6 months. So as a prescriber, it is important to put a stop date/plan GC tapering from the outset.
Fifth: I found the Non-immune treatment section useful in terms of nephroprotection (low salt diet, blood pressure control with RAAS-blockade and to consider adding SLGT2-I if residual proteinuria after 12 months); dyslipidaemia; vaccinations and bone health.
It might be because of the time constraint to present the recommendations at the congress, but I was puzzled to see no section pertaining to Maintenance of therapies in the summary figure. Overall, the EULAR recommendations represent a significant update and we are looking forward to reading the full guidance and implementing them to improve the care and outcomes of patients with LN.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.