DMARD Treatment Lags for Minority Groups with Rheumatoid Arthritis Save
Key Takeaways
- Racial-ethnic disparities in care quantity and quality have been well documented throughout medicine.
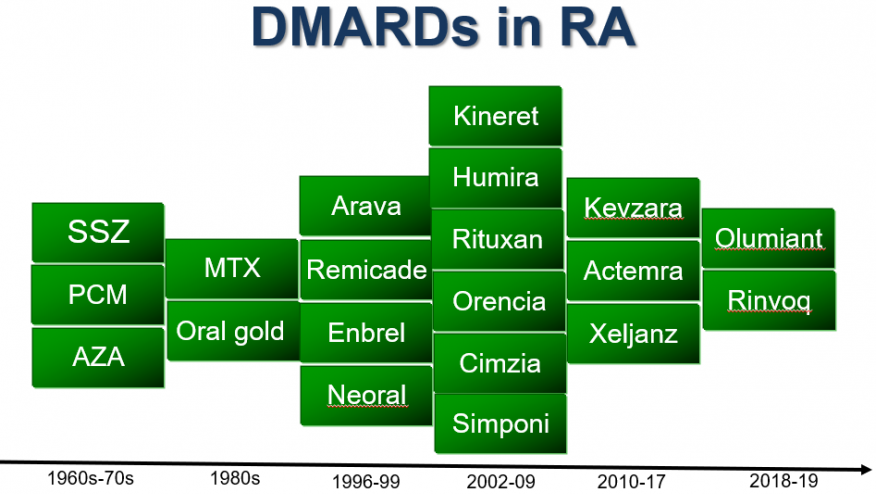
- This study focused on rheumatoid arthritis patients' use of disease-modifying anti-rheumatic drugs (DMARDs) in the U.S., examining recent federal survey data.
- It found that each major minority group had substantially lower DMARD utilization than white patients, even when adjusting for household income, education, and other sociodemographic parameters.
Use of disease-modifying anti-rheumatic drugs (DMARDs) for rheumatoid arthritis (RA) was markedly lower among all major racial-ethnic minority groups in the U.S. compared with white patients, analysis of federal survey data indicated, even after adjusting for income, education, and other factors.
Raw data from the government's Medical Expenditure Panel Survey (MEPS) showed that 23.9% of white people reporting an RA diagnosis had been taking some type of DMARD, compared with 7.9% of those identifying as Asian, 14.1% of Black RA patients, 18.8% of Hispanic patients, and 12.6% of those listed as "other/multiple" ethnicity, according to Utibe Essien, MD, MPH, and colleagues at the University of California Los Angeles.
Adjusting for sociodemographic variables reduced the disparities slightly, and further adjustment for having recent rheumatologist visits cut them a bit more, the researchers reported in a Journal of Rheumatology research letter. But while in some cases the differences were no longer statistically significant, the numerical values still pointed to substantially lower rates for the minority groups relative to white patients.
Nevertheless, Essien and colleagues were encouraged by their finding that DMARD uptake improved when patients had seen a rheumatologist. This, they wrote, "suggest[s] a potential mechanism to advance pharmacoequity in RA." Further improvements in rheumatologist access "may help mitigate these disparities," they added.
As the U.S. Agency for Healthcare Research and Quality explains, "MEPS is the most complete source of data on the cost and use of healthcare and health insurance coverage." It enrolls a new sample each year, with participants completing detailed questionnaires on healthcare encounters, diagnoses they had been given, and medications and other treatments received. Around 10,000 to 15,000 households are included each year, representing a total of some 30,000 to 35,000 individuals.
Essien and colleagues analyzed MEPS data from 2011 to 2022, identifying 6,260 individuals reporting RA diagnoses. Of these, 2,850 listed themselves as white, 1,647 as Black, 1,318 as Hispanic, 210 as Asian, and 235 as other/multiple. Mean ages in these groups ranged from 58 to 65, and 63% to 73% were women. Besides age and sex, data were also adjusted for household income, educational attainment, census region (Northeast, South, Midwest, West), insurance type, and presence of other chronic illnesses.
Rheumatologist visits were also asked in the survey. This varied considerably, although not even one-third of any group had seen one in the past year, which itself could be seen as concerning. Rates among the different groups were as follows:
- White: 31.1%
- Black: 19.1%
- Hispanic: 23.2%
- Asian: 17.2%
- Other/multiple: 24.7%
The researchers analyzed DMARDs separately for conventional agents such as methotrexate and for biologic products. For the most part, intergroup differences in use rates were smaller for conventional DMARDs versus the costlier biologics. But not in every case: Among Asian patients, point estimates for odds ratios, with whites as the reference, were actually lower for conventional DMARDs, at about 0.25 in the raw data versus approximately 0.35 for biologics. (Of course, the low rates of DMARD use in all groups -- from 76% to 92% in the five groups reported using none at all -- may raise eyebrows as well, insofar as DMARDs are the guideline-recommended foundation of RA care.)
Biologics use was far lower than for conventional agents. Rates were in the range of 2.2% to 6.3% -- highest for white patients, lowest for Black patients -- as compared with 7% to 20.4% for conventional agents. With those drugs, again the rates were highest among white patients while the lowest was in the Asian group; rates for Black, Hispanic, and other/multiple individuals ranged from 11.7% to 17.3%.
Adjusting for income, education, and other socioeconomic factors reduced the drug usage odds ratios somewhat. For example, among Black patients, an OR just below 0.6 was seen for conventional DMARDs and about 0.3 for biologics, relative to white patients. With these adjustments, these ORs rose to about 0.8 and 0.4 for conventional and biologic agents, respectively, both statistically significant. The additional adjustment for rheumatologist visits pushed the ORs for Black patients up by another 0.1 or so.
Interestingly, the disparities for Asian versus white patients remained nearly the same when the sociodemographic adjustments were taken, while they made a big difference for Hispanic patients, among whom the disparities nearly vanished. Meanwhile, the adjustment for rheumatologist visits shrank the difference considerably for Asian patients but made no impact at all for Hispanic patients.
The study's chief limitation was its reliance on respondents' recall of RA diagnoses, which were not checked against physician or hospital records. Disease severity was not asked in MEPS and therefore not taken into account. Also, the small number of Asian patients, and the even smaller numbers who used DMARDs, left the comparisons with white patients with very broad confidence intervals that crossed 1.0 for the biologics odds ratios.
On the other hand, Essien and colleagues pointed out that the MEPS data have a unique strength in that, unlike most other large datasets, it includes people without insurance and is about as representative of the U.S. population as can be.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.