Do SGLT2 and GLP-1 therapies have a role in Lupus? Save
Sodium-Glucose Cotransporter 2 Inhibitors (SGLT2i) and Glucagon-like peptide-1 receptor agonists (GLP1-RA) were initially developed as glucose-lowering agents for the treatment of Type 2 Diabetes. Since their introduction, they have been noted to have a myriad of other benefits, including cardiovascular and renal protective effects in patients both with and without diabetes. These benefits, along with already widespread use and generally good tolerability profile, have piqued interest in the potential benefit of SGLT2i and GLP1-RA in patients with rheumatologic conditions, who are at higher risk of cardiovascular and renal complications.
Here, we will review the evidence for SGLT2i and GLP1-RA in lupus.
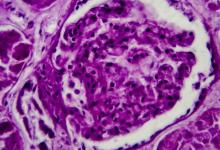
One of the most common and devastating severe manifestations of SLE is lupus nephritis (LN), which affects an estimated 40-70% of lupus patients. Mortality associated with lupus is significantly higher in those with LN compared with those without LN, and death directly attributable to kidney disease occurs in 5% to 25% of patients with proliferative LN within 5 years of onset. Ultimately, 10% to 30% of patients with LN progress to end stage renal disease requiring renal replacement therapy even with our current immune targeted therapies1,2.
Thus, there is great interest in optimizing or generating alternative treatments for the many LN patients that fail to respond fully to current therapies. Importantly, current therapeutic approaches focus on alleviating immune-mediated injury to the kidney, mainly targeting the migratory and functional features of immune cells with little impact on fibrosis or chronicity. Immune activation in the kidney can lead to a cascade of tissue injury, in part via contributing to a hypoxic environment. Tissue hypoxia and oxidative stress also can contribute to non-immune mediated tissue injury driven by renal stromal cells, further enhancing interstitial immune cell infiltration and fibrosis to create a viscous cycle3. SGLT2i are a class of drugs that we hypothesize may have a beneficial effect on these pathways 4 that are not well targeted by current treatment paradigms.
SGLT2i were initially approved for the treatment of type 2 diabetes in 2013 due to their glucose lowering effects. Importantly, multiple large randomized clinical trials have since demonstrated the remarkable effect of this class of drugs in preventing adverse renal outcomes in patients with diabetic nephropathy but also a diverse range of other chronic kidney diseases 5,6. As such, the FDA has since approved SGLT2i to reduce the risk of kidney function decline in both diabetic and non-diabetic patients with CKD.
Interestingly, these drugs also have a major benefit on cardiovascular disease outcomes and are approved to reduce major adverse cardiovascular events in type 2 DM patients with CV disease and independently in heart failure patients. Thus, SGLT2i have become a mainstay of chronic kidney disease (CKD) and congestive heart failure treatment. These large studies on SGLT2 inhibitors have largely excluded patients with autoimmune diseases due to concerns for confounding from immunosuppression. Nevertheless, the widespread benefits of SGLT2i have raised interest in their therapeutic potential in lupus, with promising initial safety and efficacy data in small studies. In a mouse model of LN, SGLT2i were shown to alleviate podocyte damage via mTORC1 and autophagy pathways7. We have further demonstrated that SGLT2i have an anti-fibrotic effect in the lupus mouse kidney and surprisingly also reduce autoreactive plasma cells and autoantibodies, possibly via altering oxidative stress. A phase I/II trial of dapagliflozin in 38 lupus patients (including with and without lupus nephritis) showed an acceptable safety profile, with no increase in disease activity or proteinuria over the 6 months of the study. Another two small studies (with n=5 and n=9, respectively) demonstrated that SGLT2i decreased proteinuria in LN. Finally, a retrospective cohort study compared 1775 matched pairs of SGLT2i users and nonusers with SLE and type 2 diabetes from the TriNetX database and found that use of SGLT2i was associated with significantly reduced risk of lupus nephritis, dialysis, kidney transplant, heart failure, and all-cause mortality compared with no SGLT2i use 8 9,10.
While GLP1-RA have been suggested to have disease modifying properties in other autoimmune diseases such as psoriasis and psoriatic arthritis, modulating inflammatory pathways independent of their weight-reducing effects11, there is very little data on GLP1-RA in lupus. There is considerable evidence that GLP1-RA confer cardiovascular and renal protective effects in patients with and without diabetes12. Given higher rates of cardiovascular and renal complications in lupus patients relative to the general population, lupus patients certainly stand to particularly benefit from GLP1-RA if they are proven safe in this patient population. A retrospective study of patients in the NYU Lupus Cohort found that GLP1-RA use was associated with significantly decreased BMI and did not confer a higher risk of flares, though notably the sample size was small13. Furthermore, a retrospective study using TriNetX found that treatment with a GLP1-RA at any point following a LN diagnosis reduced the 5-year rate of progression to ESRD by half14. On the other hand, there have been some case reports of drug-induced lupus associated with GLP1-RA use, in particular with semaglutide, so further study is warranted15.
In summary, there is substantial mechanistic rationale for the benefit of SGLT2 inhibitors and GLP1-RA in lupus. Indeed, small studies have demonstrated that SGLT2 inhibitors can be utilized safely and efficaciously in patients with lupus nephritis, though with fewer studies on GLP1-RA. Additional research is needed to identify where these medications fit into the rheumatology treatment armamentarium and their precise mechanisms of action.
Supported by a Lupus Mechanisms and Targets Award from the Lupus Research Alliance
References
1. Morales, E., Galindo, M., Trujillo, H. & Praga, M. Update on Lupus Nephritis: Looking for a New Vision. Nephron 145, 1-13 (2021).
2. Mahajan, A., et al. Systemic lupus erythematosus, lupus nephritis and end-stage renal disease: a pragmatic review mapping disease severity and progression. Lupus 29, 1011-1020 (2020).
3. Davidson, A. What is damaging the kidney in lupus nephritis? Nat Rev Rheumatol 12, 143-153 (2016).
4. Bessho, R., et al. Hypoxia-inducible factor-1alpha is the therapeutic target of the SGLT2 inhibitor for diabetic nephropathy. Sci Rep 9, 14754 (2019).
5. Heerspink, H.J.L., et al. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med 383, 1436-1446 (2020).
6. Wiviott, S.D., et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med 380, 347-357 (2019).
7. Zhao, X.Y., et al. SGLT2 inhibitors alleviated podocyte damage in lupus nephritis by decreasing inflammation and enhancing autophagy. Ann Rheum Dis 82, 1328-1340 (2023).
8. Morales, E. & Galindo, M. SGLT2 inhibitors in lupus nephropathy, a new therapeutic strategy for nephroprotection. Ann Rheum Dis (2022).
9. Wang, H., et al. Safety and efficacy of the SGLT2 inhibitor dapagliflozin in patients with systemic lupus erythematosus: a phase I/II trial. RMD Open 8(2022).
10. Yen, F.S., Wang, S.I., Hsu, C.C., Hwu, C.M. & Wei, J.C. Sodium-Glucose Cotransporter-2 Inhibitors and Nephritis Among Patients With Systemic Lupus Erythematosus. JAMA Netw Open 7, e2416578 (2024).
11. Karacabeyli, D. & Lacaille, D. Glucagon-Like Peptide 1 Receptor Agonists in Patients With Inflammatory Arthritis or Psoriasis: A Scoping Review. J Clin Rheumatol 30, 26-31 (2024).
12. Badve, S.V., et al. Effects of GLP-1 receptor agonists on kidney and cardiovascular disease outcomes: a meta-analysis of randomised controlled trials. Lancet Diabetes Endocrinol 13, 15-28 (2025).
13. Carlucci, P.M., et al. A retrospective evaluation of glucagon-like peptide-1 receptor agonists in systemic lupus erythematosus patients. Rheumatology (Oxford) 64, 3085-3089 (2025).
14. Palmer, A. & Tan, I. Risk of End-Stage Renal Disease Among Patients with Lupus Nephritis on GLP-1 Receptor Agonists: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol 76(2024).
15. Castellanos, V., Workneh, H., Malik, A. & Mehta, B. Semaglutide-Induced Lupus Erythematosus With Multiorgan Involvement. Cureus 16, e55324 (2024).








If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.