Mimics of ANCA-associated vasculitis: How can we tell? Save
With increased disease awareness and more regular, accessible testing for anti-neutrophil cytoplasmic antibodies (ANCA), ANCA-associated vasculitis (AAV) has become an increasingly recognized clinical entity in rheumatologic practice.
While a number of classical paradigms of presentation are recognized, such as abrupt pulmonary-renal syndrome in microscopic polyangiitis or recurrent, non-infectious sinus inflammation in limited granulomatosis with polyangiitis, this group of diseases remains heterogeneous with a vast spectrum of clinical presentation. This poses a unique challenge to clinicians when pinning down the diagnosis, especially when considering “mimicking” conditions that may present similarly but require markedly different treatment approaches. In the case of AAV, frequently considered mimics are infections (especially infective endocarditis), medication-induced vasculitis (ie hydralazine), and substance-induced vasculitis (most often cocaine/levamisole-related).
When time-sensitive treatment is often needed for AAV to prevent organ-threatening complications, what clues can we use to determine if a mimicking condition might be present? Vural et al. sought to answer this question in Abstract #713 titled “Differentiating ANCA associated vasculitis from Secondary forms”.
The group retrospectively reviewed the charts of patients with glomerulonephritis from infective endocarditis, drug-induced AAV, or primary AAV in order to compare and contrast features which may distinguish the entities. In total they reviewed 42 cases of glomerulonephritis due to infective endocarditis, 35 cases due to drug-induced AAV, and 50 cases due to primary AAV. Of infectious cases, bartonella was the most common pathogen occurring in just over half of these patients. Of the drug-induced cases, almost all were linked to hydralazine use.
Leukopenia and thrombocytopenia were far more common in infectious and drug-induced cases compared to leukocytosis and thrombocytosis in primary ANCA vasculitis. Rates of double stranded DNA and cryoglobulin positivity were higher in secondary causes compared to primary ANCA vasculitis. Rheumatoid factor was more common in infectious endocarditis cases (64%) though interestingly, still fairly present in primary cases (37%). As has been previously reported, primary ANCA vasculitis cases experienced a high concordance of ANCA IF and antigen (94%) compared to drug-induced cases (60%) and infectious cases (40.5%). Hypocomplementemia was more frequent in secondary causes.
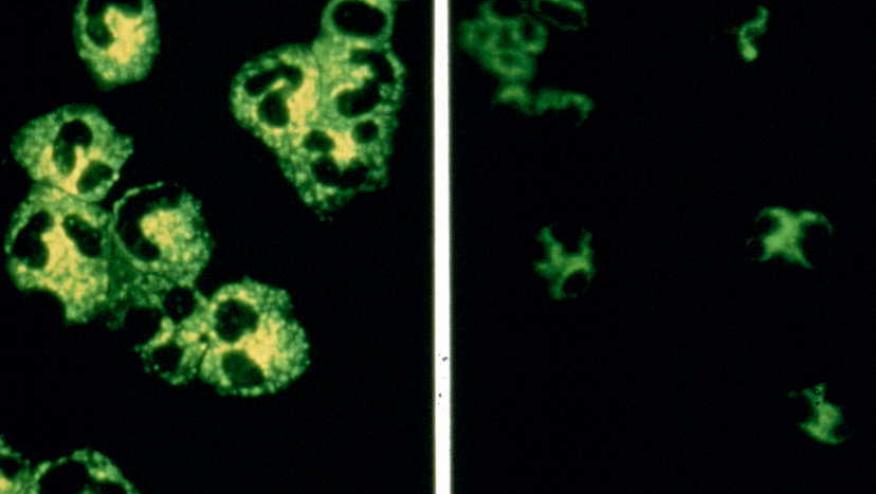
When renal biopsies were examined, all primary ANCA vasculitis cases had histology most consistent with pauci-immune glomerulonephritis, and they very rarely exhibited any immunofluorescence. Drug-induced vasculitis cases were also felt to be consistent with pauci-immune glomerulonephritis but started to more frequently immunofluorescence positivity (10-35% depending on targeted stain). Infective endocarditis cases exhibited the most immunofluorescent positivity and histology more often showed immune complex glomerulonephritis (55%) compared to pauci-immune glomerulonephritis (45%).
Dialysis cessation occurred most frequently in primary AAV patients (75%) followed by infective endocarditis cases (30.7%) and then by drug-induced cases (18.7%). Six month mortality was higher in cases due to secondary causes.
This abstract emphasizes important clues in differentiating primary AAV from secondary infective endocarditis or drug-induced causes, namely the presence of high/low platelets and leukocytes, ANCA discordance, other autoimmune labs, and renal biopsy features. This study demonstrated etiology is helpful in prognosticating these patients, both from a renal recovery as well as a mortality standpoint.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.