Putting IL17i into ‘focus’ for SpA-associated uveitis Save
The longest studied drug for uveitis in SpA has been monocolonal TNFi Abs. Reductions of acute anterior uveitis have been found with etanercept but less impressively than adalimumab, infliximab, and in my opinion less than golimumab and certolizumab pegol.
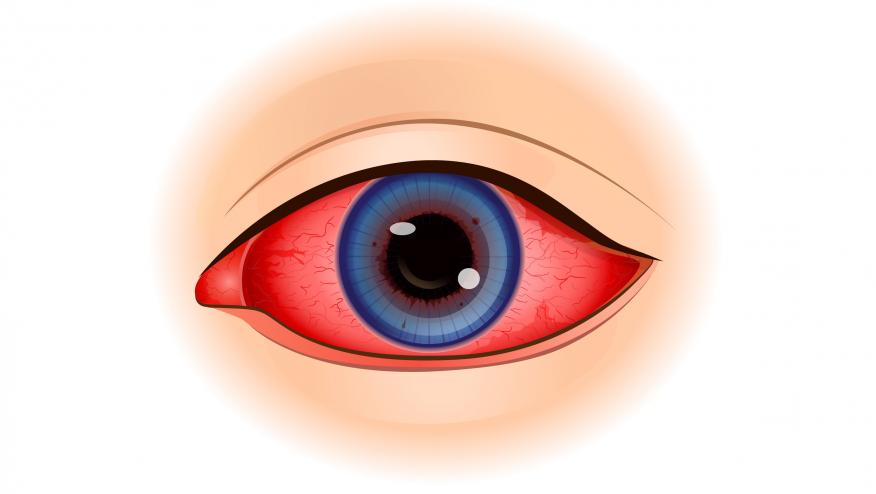
Other data have emerged for JAKi and IL17i, with respect to acute anterior uveitis. IL-17A and IL-17F have been found in anterior uveitis (1).
Brown et al (1) determined the rates of uveitis in a post hoc analysis of SpA RCTs (phase 2b/3).
In 2 phase 3 studies (BE MOBILE 1 and 2), uveitis was reduced in bimekizumab pts vs placebo 1.8/100 patient years (PYs) (0.2 to 6.7) vs 15.4/100 PYs and uveitis occurred in 0.6% (2/349) of BKZ pts vs 4.6% (11/237) in placebo. The pooled incidence was reduced at 1.2/100 PYs.
If there was a history of uveitis, again bimekizumab seemed protective (bimekizumab 6.2/100 PYs vs. placebo 70.4/100 PYs).
Data presented at EULAR showed lower rates of uveitis also in PsA with bimekizumab (and they used the pooled data also from the PsA studies). Uveitis is less frequent in PsA than axSpA and the former is often post uveitis, bilateral whereas in axSpA it is often acute anterior unilateral uveitis (2).
Whether IL17A and F inhibition is different from IL17Ai is yet to be determined as there are no head to head studies (3). However, in my opinion, the initial gold standard Rx for frequent recurrent uveitis in axSpA would be a monoclonal TNFi Ab but IL17is can be considered and thus far, the largest dataset with statistically significant differences may be from bimekizumab.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.