Emergencies, Independence & Hemorrhage (1.23.2026)
Dr. Jack Cush reviews the news and reports from the past two weeks on RheumNow.Com
Read Article

Links:

Links:
Dr. Jack Cush reviews the news and reports from the past two weeks on RheumNow.Com
Read Article

Links:

Dr. Jack Cush reviews the news and journal reports from RheumNow.com, including info on scleroderma, dermatomyositis and malignancy, rheumatologist and APP salary concerns.
Read Article



Links:

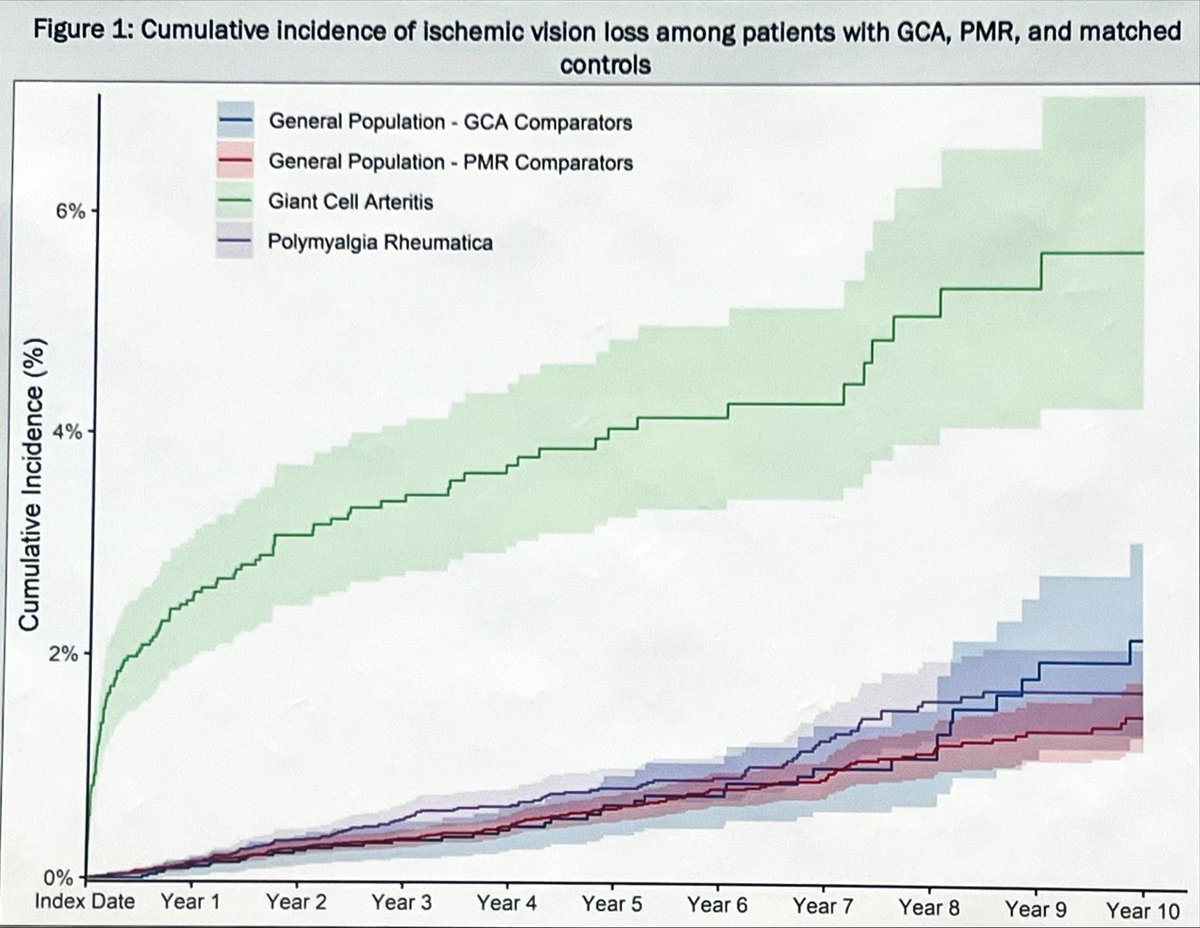

Jiha Lee @JihaRheum( View Tweet )


Dr. Jack Cush reviews the news and journal reports from the past week on RheumNow.com. Are there benefits to diet or vegan diets? What's the effect of menopause on CTD? Ro52 makes a big entrance with all our ILD coverage this month.
Read Article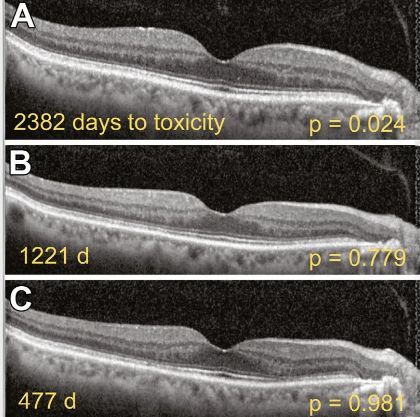
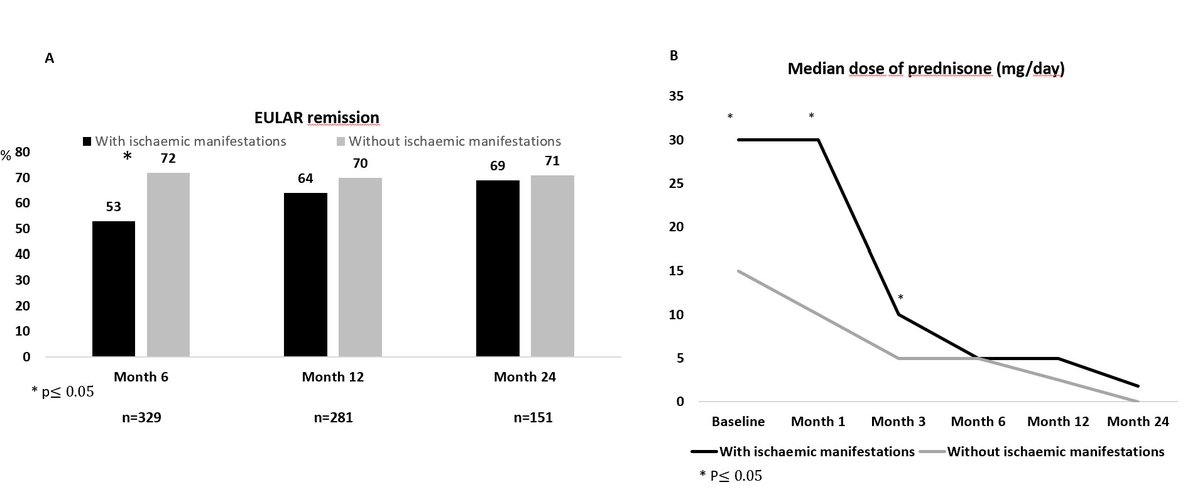
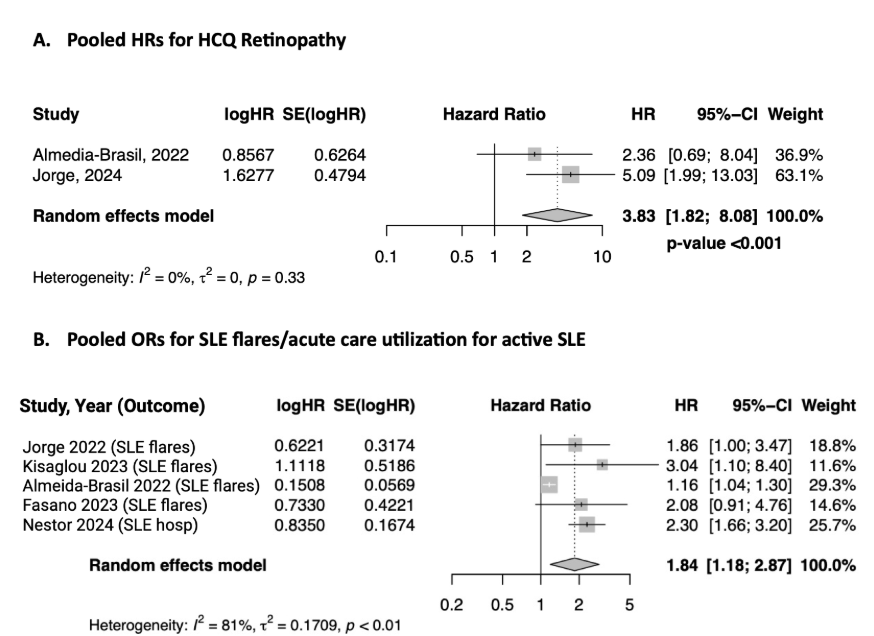
We review the available literature, with a particular focus on the recent findings in the Hopkins Lupus Cohort, regarding the clinical utility of hydroxychloroquine blood levels in helping to clarify some of the issues regarding retinopathy, how best to dose this medication, and medication adherence.
Here are five things every rheumatologist should know about antimalarial medications for lupus.
By downloading this material, I acknowledge that it may be used only for personal use and personal education and that I will accredit RheumNow.com as the source and owner of this material. Commercial use or mass reproduction of this material without permission from RheumNow (info@rheumnow.com) is prohibited.