Rheumatology Workforce: Is it a Women’s Issue? Save
In 2021, the Association of American Medical Colleges estimated a physician workforce shortage by 2024 of between 37,800 and 124,000 across all specialties. The American College of Rheumatology has been looking at workforce projections in both adult and pediatric rheumatology for nearly a decade, and in 2015 published the “2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015–2030”. These projections, which look at distributions of rheumatologists and advanced practice providers in clinical care in both private practice and academic institutions, found:
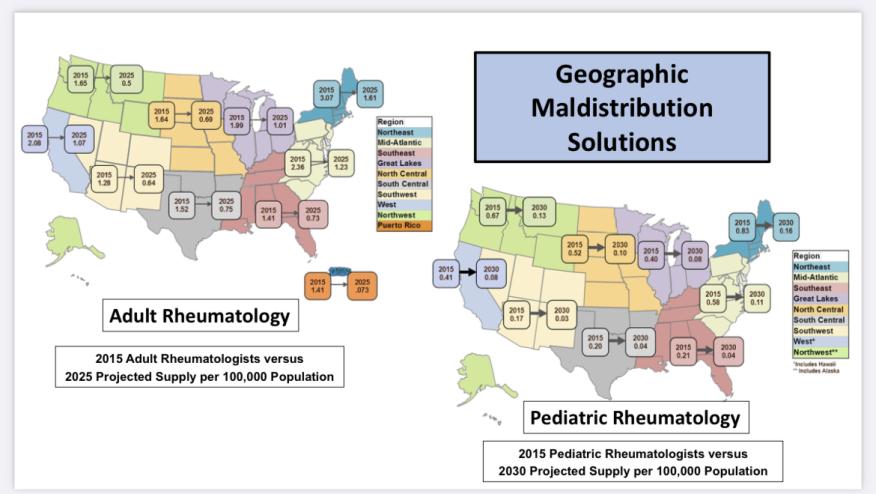
- An estimated 6,013 rheumatology providers were currently in practice (including physicians, nurse practitioners, and physician’s assistants). The report estimated demand will exceed supply by 4,133 clinical full-time employees in 2030, with a geographic/regional maldistribution. The greatest concentration of rheumatologists/APPs is in the Northeast, Mid-Atlantic, Midwest/Great Lakes, and California West Coast.
- The pediatric workforce study from 2015 estimated 300 providers nationwide with a projected demand increase of 100% by 2030.
I recently sat down with Dr. Daniel Battafarano, chair of the ACR’s Workforce Solutions Committee, to discuss these findings and their impact on the next few years.
In regard to the shortage, the 2015 committee was able to determine an ideal ratio of 1.6 adult rheumatologists per 100,000 in every region with the original 2015 study showing all regions below 1.0 except the Northeast at 1.61 in 2025. The ratio projections were less clear for pediatric rheumatology, but every region showed severe shortages in 2015. Things are predicted to be worse by 2030.
Unfortunately, no one anticipated the COVID-19 pandemic and its effect on the workforce.
“The pandemic definitely accelerated workforce shortages that were difficult to measure nationally or regionally. It (the pandemic) accelerated retirement for some rheumatologists who were in private business practices. All rheumatologists lost income for their businesses and their employees for months, and some decided to retire earlier than previously planned.
Furthermore, approximately 50% of rheumatologists are women and the pandemic affected their professional and personal responsibilities. Many chose to decrease their workload in rheumatology to offset childcare challenges and online schooling requirements. After the pandemic slowed, many women rheumatologists have been unable to return to their previous clinical FTEs due to ongoing responsibilities and quality of life issues.”
Given additional, currently unknown workforce issues, the continued work of the committee focuses on the future.
“In 2022, the Northwest, the Southwest, and the South Central regions were identified as three primary regions in the U.S. most in need of regional rheumatology workforce solutions. These regions also have a paucity of rheumatology fellowship training programs despite having excellent medical universities and medical centers. The ACR and the Rheumatology Research Foundation committed to address workforce solutions in these areas,” Dr. Battafarano shared.
In particular, this commitment entails implementing five primary overarching interventions in these regions, including three training strategies and two business strategies:
1) Initiate new and innovative rural ACGME fellowships and optimize rheumatology training of advanced practice providers (APPs) in these underserved regions bridging rheumatology care into primary care clinic networks with telemedicine.
2) Facilitate recruitment opportunities to sustain the regional workforce with financial incentives, loan repayment, end-of-career retirement strategies, and financial support for telemedicine and multistate licensing.
3) Foster patient-centered care with regional/community stakeholders including insurers and facilitate health care delivery models, where possible, for value-based care with direct access to interdisciplinary care.
4) Provide practical, virtual rheumatology training modules for primary care providers and APPs including physical therapists, occupational therapists, and doctors of pharmacy (PharmD) to expand the rheumatology health care network.
5) Identify education and grant support for education/training and clinical research.
“These ACR workforce solutions may be implemented alone or promoted in combination for underserved communities in these regions. It is anticipated that the success and experience of these interventions in the Northwest, Southwest and South Central regions will enable future success for other regions in the U.S."
Dr. Battafarano reflected that this arguably is a “workforce that significantly impacts women”. While approximately 50% of physicians are female (among advanced practice providers, the number is higher), this number is expected to increase in the coming years. The current primary workforce interventions are not fully representative of this highly female-represented workforce. This should be our call to action to find flexible solutions that truly reflect the current and projected needs for our workforce.
The ACR Workforce Solutions Committee needs more volunteers, and Dr. Battafarano encourages interested individuals to contact Connie Herndon, ACR Vice President, Research, Training and Workforce.
1. AAMC Report Reinforces Mounting Physician Shortage
2. Battafarano DF, Ditmyer M, Bolster MB, Fitzgerald JD, Deal C, Bass AR, et al. 2015 American College of Rheumatology Workforce Study: Supply and Demand Projections of Adult Rheumatology Workforce, 2015-2030. Arthritis Care Res (Hoboken). 2018;70(4):617-26.
3. Correll CK, Ditmyer MM, Mehta J, Imundo LF, Klein-Gitelman MS, Monrad SU, et al. 2015 American College of Rheumatology Workforce Study and Demand Projections of Pediatric Rheumatology Workforce, 2015-2030. Arthritis Care Res (Hoboken). 2022;74(3):340-8.
4. The Physicians Foundation. 2021 survey of America’s physicians COVID-19 impact edition: a year later; 2021.
Join The Discussion
Flexibility concerning our workforce shortage is needed as well as creativity. Sharing job opportunities for physicians and use of Advance Providers will be imperative. Looking to the future for health care will be daunting but achievable.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.