Vasculitis Save
Sunday’s vasculitis session at RNL26 was a fantastic update on inflamed blood vessels, large and small, by two experts in the field.
Mike Putman, MD, started us off by provocatively inviting us to embrace relapse in GCA and PMR. Dr. Putman started by taking us through the traditional state of play. Standard of care approach in PMR (with no flares!) being to give 1890mg prednisone over 43 weeks. This is a lot! And many regimes give even more base steroid, and if flares happen, as they do, even more steroid results. There is a common misconception among patients, I think often fostered by attempts at reassurance by clinicians, that PMR will be cured with a year of steroid. This is just not true, and Dr. Putman described how ¾ of patients are still on steroids at 1 year, ½ still on steroids at 2 years, and ¼ still on steroids at 5 years.
We now have trials of rituximab, tocilizumab, sarilumab, and secukinumab showing good efficacy in PMR, albeit the first was a small study with surprising results that needs replication and the last is only a press release to date. Certainly for IL-6i at least however, the data supports convincing efficacy. Dr. Putman went on to propose a new paradigm for PMR treatment. This emphasises a more rapid steroid taper, with those who can getting off steroids quickly, and those who can’t, starting a biologic DMARD early. Both facets of this approach aim at steroid minimisation, which I think we all can agree, is a good thing.
Dr. Putman then proceeded to teach us some lessons from recent trials of GCA. These have clearly demonstrated that tocilizumab and upadacitinib are highly effective agents in GCA, and there is a very good argument that one should be given to all patients (who don’t have contra-indications). We fear vision loss in GCA given its generally complete and irreversible nature. However, Dr. Putman demonstrated from the trial data that vision loss is very rare in the modern era once therapy has commenced with 2 cases in 859 patients across the trial programmes. Dr Putman finished by advocating for more rapid steroid tapers in GCA similar to those used in the clinical trials. This approach along with the significantly lower relapse rate in those on bDMARDs will result in a far lesser burden of steroid related adverse events in the long term. We do have some self-improvement work to do in order to overcome our historical fear of the ischaemic complications of GCA to achieve this laudable goal.
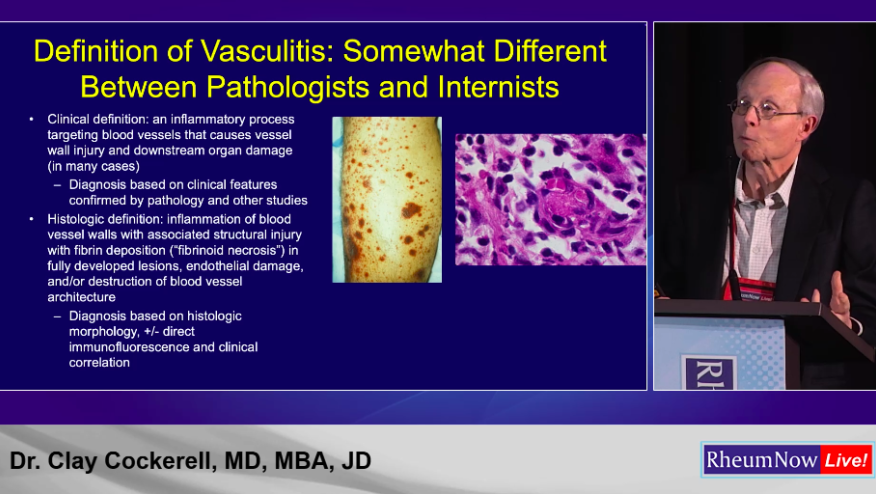
Cutaneous vasculitis is generally the most visible manifestation of systemic vasculitis. In common with many dermatologic conditions however it remains somewhat of a confusing area for many rheumatologists. Clay Cockerell, MD, MBA, JD gave us all a dermatologic tour de force with a wealth of fantastic clinical and histologic images. There were a few key clinical points and nuances that I took from this talk.
Dr. Cockerell’s first few points coalesced around the fact that clinicians and pathologists are often speaking a different language when it comes to vasculitis and its associated findings. This can lead to difficulties both in interpreting pathology reports and also in providing the pathologist with sufficient clinical information to make an informed report. This is something that can only be improved by building closer working relationships with our pathology colleagues.
Dr. Cockerell went on to discuss urticarial vasculitis, a relatively common suspected referral we receive, that rarely translates into a confirmed diagnosis. He emphasised that clinical features such as duration of urticaria and bruising may be relatively unreliable in supporting urticarial vasculitis as the aetiology of urticaria due to issues with recall and scratching. Therefore, serologic markers such as low complement levels may be more reliable predictors.
Dr. Cockerell went on to emphasise how crucial timing of the biopsy is where direct immunofluorescence is concerned. Ideally this is performed on fresh lesions within 24 hours, otherwise the sensitivity drops significantly and false negatives abound.
Overall the underlying messages here where an emphasis on close collaboration with our dermatology and pathology colleagues, and perhaps a gentle chiding to us all to try and improve our dermatological clinical skills and knowledge of the nuances of skin biopsy.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.