All News
Links:

Caoilfhionn Connolly CaoilfhionnMD ( View Tweet)
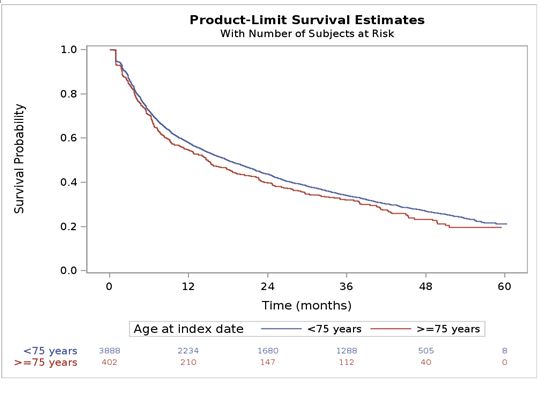
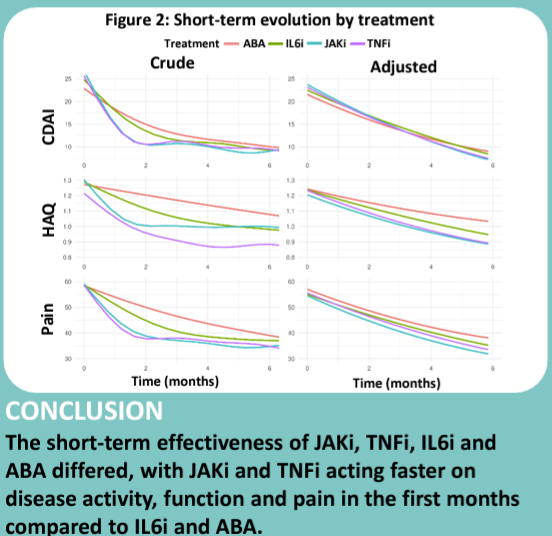
Older adults with RA receive less DMARDs, the standard of care. Dr. Bruno Fautrel shows TOC tolerance in older adults is comparable to younger patients. Let's treat the patient, not their age! #ACR24 @RheumNow ABST#0516 https://t.co/054RWGh3a7

Bella Mehta bella_mehta ( View Tweet)
Links:
Links:

Antoni Chan MD (Prof) synovialjoints ( View Tweet)

Caoilfhionn Connolly CaoilfhionnMD ( View Tweet)

Akhil Sood MD AkhilSoodMD ( View Tweet)
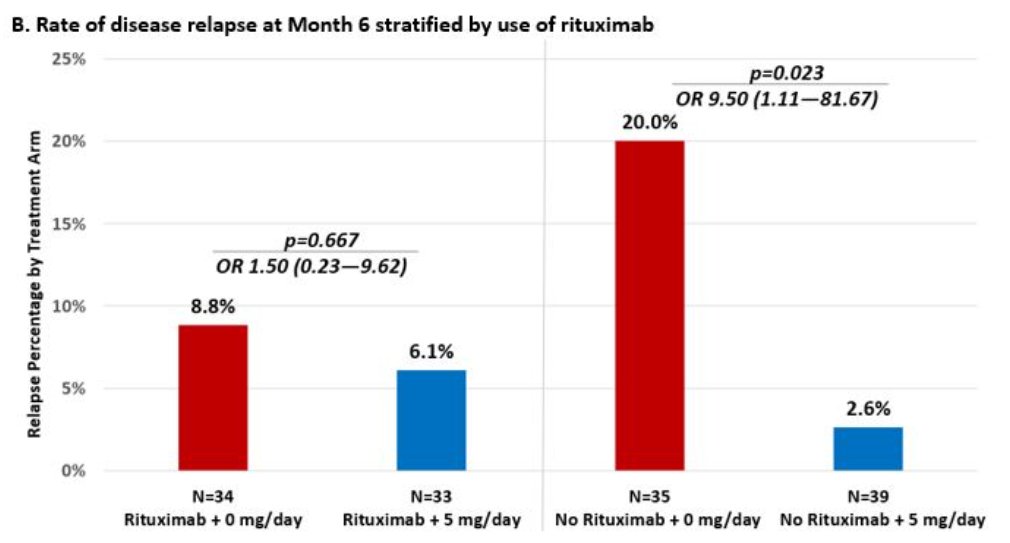
TAPIR study of continuing vs stopping steroids in ANCA vasculitis in remission. Relapse at month 6 in 16% vs 4%. OR 4.22, but low rate in either group. If treated Rituximab, no difference! Merkel et al. @RheumNow #ACR24 Abstr#0774 #ACRbest https://t.co/pKa4U5L2fW https://t.co/MjzE14SeGi
Links:

Eric Dein ericdeinmd ( View Tweet)
Links:

Akhil Sood MD AkhilSoodMD ( View Tweet)

Akhil Sood MD AkhilSoodMD ( View Tweet)

Caoilfhionn Connolly CaoilfhionnMD ( View Tweet)



