All News

Which CAR-based strategies would you consider to treat severe refractory #SLE based on data presented at #EULAR2025? @RheumNow
Md Yuzaiful Md Yusof Yuz6Yusof ( View Tweet)

POETYK PsA-1
Deucravacitinib TYK2i RCT Ph 3
ACR 20 DEU 54% vs. 34% PBO wk 16
ACR 50 DEU 23% vs. 14% PBO
also significant diff for HAQ-DI PASI 75 SF-36 PCS and MDA
Less Rx progression
@RheumNow #EULAR2025 LB0001 https://t.co/oRLlHwI4Bh
Aurelie Najm AurelieRheumo ( View Tweet)

Why do we need RA treatment recommendation updates? We keep on getting new data, for our keystone disease
so today Josef Smolen and colleagues present the new 2025 EULAR recommendations
#EULAR2025 @RheumNow https://t.co/OdHL8CAIKv
David Liew drdavidliew ( View Tweet)

#ClinicalPearls
For
#cartilage #swelling in #relapsing #polychrondritis
Ask for #pics
#Levamisole in #cocaine
#infection - uncommon - from piercing
Acute #bacterial v chronic
#lymphoma
#malignancy
#vasculitis
#Trauma
Hx, duration, fever can be helpful
#EULAR2025
@RheumNow https://t.co/X2b6VHYsYa
Links:
Janet Pope Janetbirdope ( View Tweet)

RCT of a digital intervention in RMDs? It was long awaited, and all the lights are green🟢!
German national Bechterew-App RCT of
App based intervention AXIA, control group was standard of care
200pts 12wks
ASAS20 response 51% vs. 9%
ASAS40 response rate 23% vs. 3%
BASDAI:
Aurelie Najm AurelieRheumo ( View Tweet)

1st #recommendations for
#Hemochromatosis #arthropathy
#psuedogout
#CPPD
#calcium #pyrophosphate #arthritis
#EULAR2025 #Recommenadations II
@RheumNow @eular_org https://t.co/AnE4T2wYoa
Janet Pope Janetbirdope ( View Tweet)

67% of HCPs knew of EULAR’s CVD risk guidelines in RMDs—but few could apply them.
✅ Only 13% linked SLE control to CVD risk
🚫 0% picked correct BP/statin use in RA/AS/PsA
Barriers? Time, knowledge, and local guideline gaps.
POS0410-HPR @RheumNow #EULAR2025
Jiha Lee JihaRheum ( View Tweet)
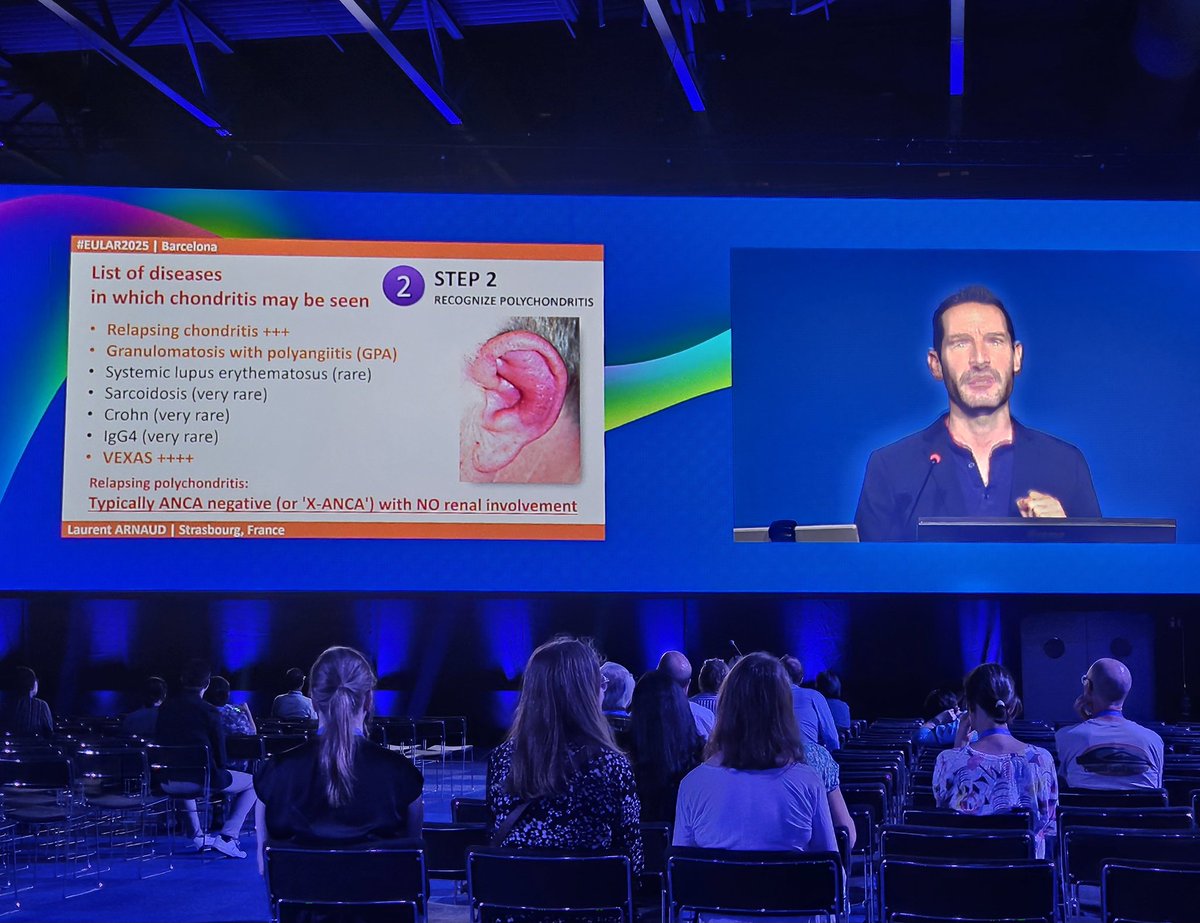
#Relapsing_Polychondritis
Main differential diagnosis is GPA
🔺️No ANCA and no renal involvement in relapsing polychondritis
@Lupusreference
#EULAR2025
@RheumNow https://t.co/QUJZ3EDjj3
Nelly ZIADE 🍀 Nellziade ( View Tweet)

“That is why this task force continues to say: nothing is better than methotrexate and glucocorticoids to start”
- Josef Smolen, on RA treatment
#EULAR2025 @RheumNow https://t.co/AbkgWS8tvH
Links:
David Liew drdavidliew ( View Tweet)

The key changes for the new 2025 EULAR recommendations on RA treatment
#EULAR2025 @RheumNow https://t.co/dp5LnoFdpW
David Liew drdavidliew ( View Tweet)

#EULAR new #RA #recommendations
J Smolen presents justification for
#MTX +#glucocorticoids at onset
do you agree?
Diff from #ACR
#EULAR #Recommendations II
#EULAR2025 @RheumNow https://t.co/wqCX5HA87q
Janet Pope Janetbirdope ( View Tweet)

URAT1 inhibitors look like the way to go in Gout!
Presented in multiple abstracts at #EULAR2025
Pozdeutinurad Ph2 long term safety data chronic gouty arthritis + tophi OP0300
Ph3 RCT of Ruzinurad in hyperuricemia/primary gout OP0302
Ph 2b RCT of SAP-001 Refractory Gout +/-
Aurelie Najm AurelieRheumo ( View Tweet)

EULAR Points to consider for the definition of #D2M #Psoriatic_Arthritis
1️⃣ Failure >= 2 b/tsDMARDs with >=2 different MOA
2️⃣ Perceived as problematic
3️⃣ Evidence of persistent disease (active disease, EMM, inflammation)
#EULAR2025
@RheumNow https://t.co/69nFEYntF0
Nelly ZIADE 🍀 Nellziade ( View Tweet)

EULAR PtC for the definition of #TR (Trt Refractory) #Psoriatic_Arthritis
#D2M
1️⃣ Failure >= 2 b/tsDMARDs
2️⃣ Problematic
3️⃣ Evidence of persistent disease (inflammation is mandatory)
+
4️⃣ Exclude comorbidities, psychosocial factors, failure due to SE/CI
#EULAR2025
@RheumNow https://t.co/8nx26mWX3C
Nelly ZIADE 🍀 Nellziade ( View Tweet)

@RheumNow When it comes to ORAL Surveillance and the 2025 EULAR recommendations, the same sensibility remains.
Appropriate caution based on the RCT, despite observational data, but we’ll see what is yet to come. Plenty to watch this space for
#EULAR2025 @RheumNow https://t.co/fIxHRGDFcK
Links:
David Liew drdavidliew ( View Tweet)

Deucravacitinib, the first oral TYK2 inhibitor, delivers in PsA:
✅ ACR20: 54% vs 34% (placebo)
✅ Skin, joints, fatigue, QoL
📉 Post hoc: less radiographic progression
No new safety signals at W16.
LB0001 @RheumNow #EULAR2025
Jiha Lee JihaRheum ( View Tweet)

📊 In POETYK PsA-1, deucravacitinib (TYK2i) significantly improved ACR20 at W16 (54% vs 34% placebo) in bDMARD-naive PsA.
Also improved QoL, skin, and MSK outcomes.
Post hoc: slowed radiographic progression.
Well tolerated & no new safety signals
@RheumNow #EULAR2025 #LB0001
Mrinalini Dey DrMiniDey ( View Tweet)

📱 Axia, a digital therapeutic for #axSpa, led to significant improvements in BASDAI, BASFI & ASQoL in a 12-week RCT.
ASAS20: 51% vs 9%; ASAS40: 23% vs 3%.
Promising app-based intervention comprising individualised exercise, pt education & disease Mx.
@RheumNow #EULAR2025 #LB0002
Mrinalini Dey DrMiniDey ( View Tweet)

from Rituximab to BiTES to CAR T, always looking for deeper B cell depletion
Safety data from CC312 CD19/CD3/CD28, a triple engager in refractory moderate-to-severe SLE
So far so good but how far do we need to go?
#EULAR2025 @RheumNow LB0007
Aurelie Najm AurelieRheumo ( View Tweet)

Older adults with chronic MSK pain report lower physical health—but better mental health—than younger peers.
Fewer missed work days, too.
Is this resilience, adaptation, or shifting expectations with age?
POS0402 @RheumNow #EULAR2025
Jiha Lee JihaRheum ( View Tweet)



