Blogs
ACR20 Pearls Part 3: Pragmatic Applications for Managing Vasculitis
While the ACR prepares to publish its new guidelines for the diagnosis and management of vasculitis in the Spring of 2020, Dr. John Stone presented his own perspectives on the practical management of vasculitis during the 2019 ACR meeting in Atlanta. He acknowledged that what may be pearls one day, may be disproven with data in the future.Steroid Poker
It began as many cases do: an ill patient, in the ICU, with signs and symptoms across several body systems, yet no clear unifying diagnosis on admission. With things stabilizing, the internal medicine hospital team on which I was serving as hospitalist that week assumed care of the patient. As the case unfolded – pulmonary infiltrates that could be hemorrhagic, renal dysfunction with proteinuria – rheumatic diseases rose in the differential. When serologic studies and other data suggested GPA rather than glomerular basement membrane (GBM) disease or other possibilities such as infection, it seemed the right time to act. And that is when a game of what I call “steroid poker” began.Remembering the Names of Drugs
Knowing the names of the agents in today’s armamentarium should be simple. But, the nomenclature is notoriously confusing. The names of monoclonal antibodies can stretch to five syllables which defy easy pronunciation beyond the “mab” at the end. Who comes up with these names anyway?When Your Patient Asks Why?
This is probably the most difficult question that a physician is confronted with. A patient is stricken with a new disease or problem and before it even sinks in or is fully comprehended, the patient wants to know “why” or “how” long before they want to know what are we can do about it.Blueprints to the Clinical Research Underworld
“If you don't know what you want, you end up with a lot you don't.” ― Chuck Palahniuk, "Fight Club" 1999
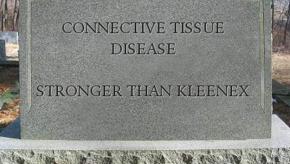
Best of 2018: Rheumatology Dead Word Cemetery 2019
I recently heard of a secondary school assignment wherein students were challenged to “bury” a word that was no longer useful or appropriate. Their exercise has now evolved into an unofficial RheumNow task force to retire diagnostic terms that have grown into misuse in rheumatology and medicine. How did we decide which words should perish? And by what criteria? Who has the final say?Best of 2018: The Delayed Diagnosis of Spondyloarthritis
You see them from the corner of your eye, standing with a kyphosis in the waiting room. They are filling out their paperwork, standing up because sitting is just not pleasant. You are the rheumatologist with an interest in ankylosing spondylitis (AS) and spondyloarthritis, so more likely than not, the patient with the bent spine is going to be your next new patient. In the back of your mind you are hoping that they are not so far along so that the therapy you may prescribe can make a difference in their life.Advice for Young Rheumatologists
You may not want my advice, but I’m going to give it to you anyway.
Pain: Objectifying a Subjective Symptom
My typically pleasant 76 year old male was livid when I walked into the exam room. He was pacing back and forth with furrowed eyebrows. I gingerly inquired what was bothering him the most.
Rheumatology Dead Word Cemetery 2019
I recently heard of a secondary school assignment wherein students were challenged to “bury” a word that was no longer useful or appropriate. Their exercise has now evolved into an unofficial RheumNow task force to retire diagnostic terms that have grown into misuse in rheumatology and medicine. How did we decide which words should perish? And by what criteria? Who has the final say?Best of 2017: Across the Table: Cush & Erkan on Antiphospholipid Syndrome
The antiphospholipid syndrome (APS) is a common disorder affecting patients with and without autoimmune disease. Despite wider recognition of APS among physicians as well as the expanding research collaborations, many clinical questions are still encountered in clinical practice, which require further evidence-based studies. In this “Across the Table” edition, Drs. Cush and Erkan discuss some of these APS-related questions. Our guest expert, Dr. Doruk Erkan offers up his approach to diagnosis and management of APS.