Anti-Phospholipid Antibodies - Infrequent in Certain Groups Save
Among patients with systemic lupus erythematosus (SLE), high titers of anti-phospholipid (aPL) antibodies were most prevalent in whites and Latinos and less so for Black and Asian individuals, researchers found.
Rates for most aPL species varied from 2% to 4% for Black patients, while they ranged up to 9% for those identifying as white or Hispanic in the study of more than 2,500 lupus patients, according to Jane E Salmon, MD, of the Hospital for Special Surgery in New York City, and colleagues.
Overall, the prevalence was 3% to 7%, the group reported in Annals of the Rheumatic Diseases.
Salmon and colleagues indicated that their "key discovery" was that clinically significant levels of anti-phospholipid antibodies were less common than might have been expected. They noted that the prevalence is "generally quoted as 25%-40%."
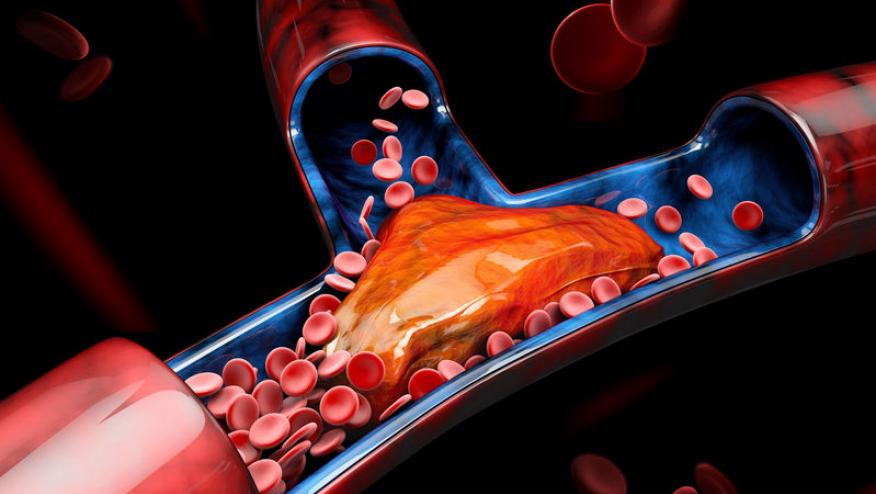
These antibodies help trigger thrombosis and serious complications of pregnancy, the researchers explained, and "can influence the course of [SLE] and contribute to organ damage." But studies of their prevalence have been marred by inconsistent methods of measurement as well as reporting. Quantitative results vary depending on which of the available assays are used; moreover, some groups have classified any non-zero finding as positive whereas others only include moderate to high titers, as those are the levels most likely to cause clinical problems.
The issue is important, though, because many other studies have found racial-ethnic variations in clinical presentations and severity of lupus manifestations, some of which might be explained by differences in aPL development.
Salmon and colleagues did not entirely get away from the latter issue. Their study used data collected from seven prospective cohorts managed by different groups -- six in the U.S. and one in France -- each of which had local laboratories handle the antibody measurement using their own methods. All, however, followed "international guidelines" in performing the tests.
For the current study, "clinically meaningful" antibody levels were defined as any of the following:
- Any presence of lupus anticoagulant (LAC)
- Moderate to high titers of anti-cardiolipin antibodies (aCL)
- Moderate to high titers of anti-β2 glycoprotein I antibodies (aβ2GPI), either IgG or IgM
Rates of LAC ranged from 14% to 20%, but despite including LAC presence in their definition of clinically significant, Salmon and colleagues then discounted it precisely because, they said, analytical methods aren't standardized. They added, too, that levels can be affected by anticoagulant medications and how samples are handled during collection and processing.
Clinically relevant aCL and aβ2GPI antibody levels were substantially less prevalent across the board. But for each, the lowest rates were in Black patients, and slightly higher among Asians. Prevalence among white and Hispanic patients was about equal. These racial-ethnic differences were statistically significant with P values ranging from 0.01 down to <0.0001.
Cohort members self-reported their racial-ethnic identities, which was an important limitation to the analysis. So was the aforementioned variability in lab testing and lack of specifics on patients' clinical conditions, other than they met official criteria for an SLE diagnosis; hence, the researchers could not try to correlate aPL titers with actual comorbidities. Also, not every member of each cohort was tested for each of the four aPL types.
"Our findings provide the impetus to discover the basis for skewed racial distribution of aPLs," the researchers concluded. "Evidence that aPLs are distributed differently among different races and ethnicities should catalyze studies to better understand the genetic and environmental factors contributing to this variability and the subphenotypes of patients with SLE."
As well, the group added, the results should inform designs of future clinical trials to ensure racially diverse enrollment. Only when trial samples "reflect real-world racial and ethnic distribution of disease" can they also account for "potential differential treatment responses."









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.