HCQ Preserves Renal Function in Lupus Nephritis Save
Key Takeaways
- While hydroxychloroquine (HCQ) helps reduce disease flares in lupus, its effect on renal function in patients with lupus nephritis (LN) is less certain.
- This study examined long-term trajectories in renal function in a retrospective chart review of more than 200 LN patients.
- When tracked for up to 10 years, declines in estimated glomerular filtration rate were significantly slower with HCQ treatment.
Lupus nephritis (LN) patients on long-term therapy with hydroxychloroquine (HCQ) showed significantly less decline in renal function, compared with patients treated otherwise, a 10-year retrospective study indicated.
Estimated glomerular filtration rate (eGFR) declines of 30% or more were 60% less likely with HCQ treatment, according to Shivani Garg, MD, PhD, of the University of Wisconsin in Madison, and colleagues. Declines of at least 40% were also 62% less likely.
The drug seemed especially protective for patients with chronic kidney disease (CKD) of grade 3 or higher, the group found, with a 77% lower risk of ≥30% eGFR decline, they reported in Arthritis Care & Research.
"[O]ur study supports the inclusion of HCQ as a pivotal component of LN management protocols, not just for its systemic benefits, but also for a potential to preserve kidney function," Garg and colleagues concluded. "These findings emphasize the importance of starting early and continuing HCQ therapy to preserve kidney health alongside overall disease control even if SLE [systemic lupus erythematosus] is limited to the kidneys."
Their study should help clear away uncertainty as to whether HCQ -- a staple of SLE therapy, but used primarily to prevent lupus flares -- also helps with LN specifically. Recent guidelines have called for HCQ to be used routinely in LN patients, but Garg and colleagues noted that this recommendation only had "modest" evidentiary support.
And, they pointed to a Chinese study from 2022 warning that HCQ actually seemed to exacerbate acute kidney injury in LN patients, which certainly complicated the issue. "Such conflicting information could potentially explain low HCQ prescribing rates (66%-79%) and even lower prescribing rates by non-rheumatologists, particularly in patients with SLE limited to the kidneys," Garg's group explained.
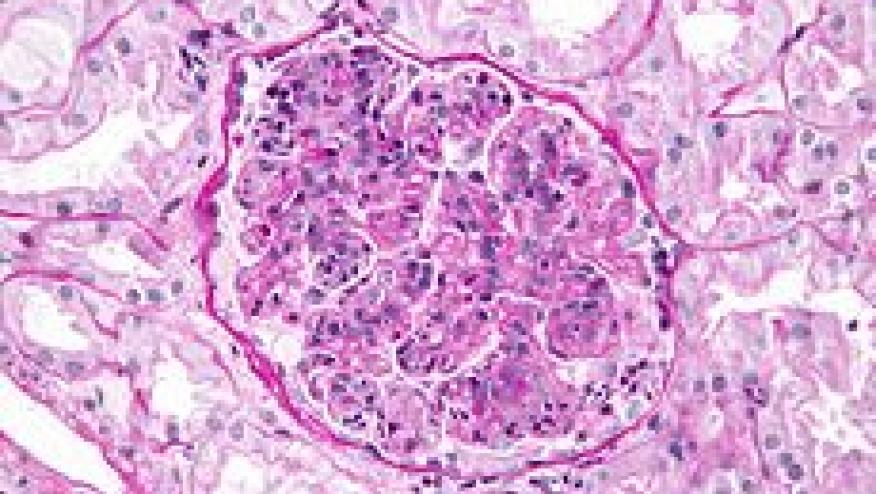
To get a better picture of HCQ's effects on kidney function in LN, they analyzed records of all patients diagnosed (and confirmed with biopsy) with LN at the University of Wisconsin's clinics from 1994 to 2019, ultimately totalling 209 patients. Of these, 79% were on HCQ at diagnosis. Use and prescribed dosage of HCQ was documented at each clinic visit, although prescriptions' duration was not; these time-varying HCQ exposures were included in the statistical modeling.
In the overall group, mean patient age was 38 at diagnosis (SD 15) and, in line with the usual sex breakdown, 75% were women. Just over a quarter had experienced SLE for at least 2 years prior to LN diagnosis. Half the group had proliferative LN, with the other half split between those with the non-proliferative form and those with a mixed presentation. At baseline, eGFR averaged 80 mL/min/1.73 m2 (SD 37). Mean follow-up was 5.4 years and ranged up to 10 years.
Certain factors predicted worse renal outcomes. With ≥30% eGFR decline as the endpoint and multivariable adjustment for demographic and clinical covariates, these included Black race (HR 4.20 vs white, P=0.0005), NIH LN Chronicity Indexo (HR 1.28 per 1-unit increment, P=0.002), and NIH LN Activity Index (HR 1.12 per 1-unit increment, P=0.005). On the other hand, some factors that might have affected eGFR trajectories seemed not to, including presence of renal arteriosclerosis, long-term use of corticosteroids, and age.
Garg and colleagues also offered a different way to view HCQ's apparent renal benefit: eGFR's graphical slope when plotted against time. Notably, HCQ users and non-users both showed mean declines. But the annual slope was less steep in users, such that over the first 5 years after diagnosis, 5.12 mL/min/1.73 m2 was "saved" each year with HCQ; over 10 years, the annual "saving" was 3.17 mL/min/1.73 m2.
As a test, the researchers also conducted the same analyses in a separate cohort of 819 patients (identified from electronic health records) with pre-existing LN. Only about one-third of this group had been using HCQ. The drug appeared to slow eGFR declines in this group, too, with an annual "saving" of 1.26 mL/min/1.73 m2.
"These findings directly address existing gaps in the literature, reduce uncertainty regarding long-term impact of HCQ use on kidney function, and highlights a benefit of early initiation of HCQ in LN, thereby empowering clinicians to advocate universal use of HCQ in LN," Garg and colleagues wrote.
Limitations included the reliance on administrative data, its sample drawn from one medical center, and lack of data on actual HCQ use as opposed to prescriptions. As well, reasons for interrupting HCQ prescribing, or never prescribing it at all, were not known.
Disclosures Garg S, et al "Hydroxychloroquine associated with lower glomerular filtration rate decline in lupus nephritis" Arthritis Care Res 2025; DOI: 10.1002/acr.25616.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.