ICYMI: How do you manage enthesitis? Save
Editor's note: This article originally appeared February 16, 2024, and is being published again this week to coincide with our Tuesday Night Rheumatology RNL Replay on Spondyloarthritis Spectrum.
Enthesitis can be a challenge for clinicians to identify, evaluate, and manage in patients with psoriatic arthritis (PsA) and axial spondyloarthritis (axSpA). It affects 27-35% of PsA patients and 36% of axSpA patients. Dr. Lihi Eder discussed the evaluation and treatment of enthesitis at RheumNow Live on January 28, 2024.
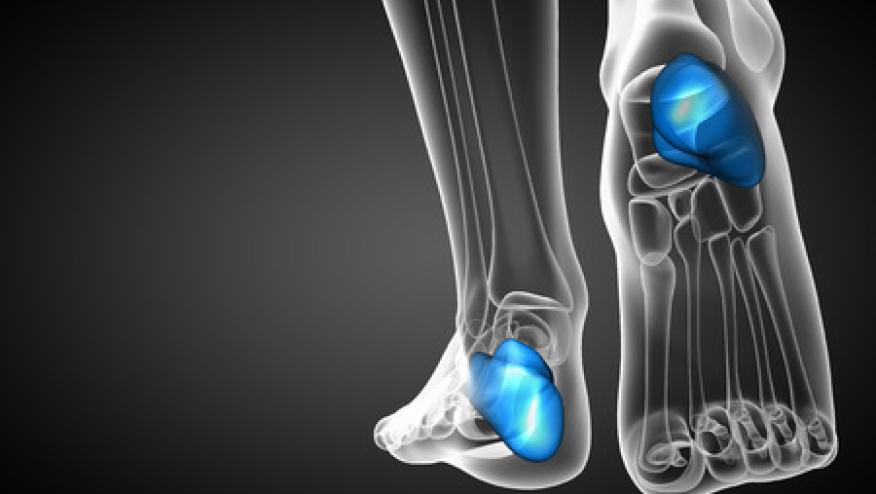
Enthesitis is caused by a local immune response to biomechanical stress and is an early finding in autoimmunity. In psoriasis patients, subclinical sonographic enthesitis is known to be common and precedes the development of PsA. Higher sonographic scores are associated with higher body mass index and nail dystrophy, common risk factors for PsA. Enthesitis is associated with higher symptom burden in PsA including more active peripheral arthritis, tenosynovitis, dactylitis, and higher pain scores. Its presence is associated with a higher risk of joint ankylosis, arthritis mutilans, peripheral joint damage and sacroiliitis.
The clinical assessment of enthesitis can be very challenging, especially on physical examination. Bedside evaluation relies upon evaluating tender entheses, as swelling is an uncommon finding. Tender entheses are non-specific and at least one tender enthesis was found in up to 50% of controls. Dr. Eder advocated adding ultrasound and other imaging modalities in this evaluation, rather than relying solely on the physical examination. Ultrasound may add to examination by assessing for hypoechogenicity, thickening, Doppler signal, erosions, and enthesophytes. These findings, however, can be non-specific and seen in patients that are older, obese, have metabolic abnormalities or have biomechanical stressors. Magnetic resonance imaging can assess for bone marrow edema and visualize deeper locations such as trochanteric and axial enthesitis. It is higher cost, however, and generally limited to particularly limited to particular locations.
The historical first-line treatment of enthesitis is non-steroidal anti-inflammatory drugs (NSAIDs), which does not have specific data for enthesitis but can be used in patients with isolated and mild enthesitis. Glucocorticoid injections can be offered, but require caution, especially around the Achilles tendon due to risk of rupture. Dr. Eder recommended using selectively and performed with ultrasound-guidance into the peritenon or bursa, and to avoid injection into the adjacent fat pad or dermis. Injections should be avoided in high risk patients who have previously had injection or have thickened tendons.
Based upon the SEAM PsA randomized controlled trial, methotrexate is conditionally recommended for enthesitis in PsA as 65% of patients in the study on methotrexate monotherapy showed resolution. All biologic therapies have shown efficacy in enthesitis including TNF inhibitors, IL-17 inhibitors, IL-12/23 inhibitors, IL-23 inhibitors, JAK inhibitors, and PDE4 inhibitors. That said, data is limited as few studies have selected enthesitis as a primary endpoint and there is limited data to suggest a difference between biologic agents. The ACHILLES study did focus upon heel enthesitis, comparing secukinumab to placebo. This showed a 42.2% resolution of enthesitis on the medication, compared to 31% with placebo representing a numerically higher, though not statistically significant benefit. One major limitation of the study was that only 56% of patients had MRI-positive enthesitis when reviewed by central reading suggesting many patients included in the study did not have active enthesitis. One study suggested benefit of IL-17 over TNF inhibition, as ixekinumab had higher resolution of enthesitis by the Spondyloarthritis Research Consortium, Canada (SPARCC), but not by the Leeds Enthesitis Index (LEI). A study looking at secukinumab versus adalimumab did not show a difference. The ECLIPSA Trial was an open-label study that showed improvement of enthesitis clearance on ustekinumab (73.9%) versus TNF inhibitor (41.7%), p=0.007. This study, however, was a non-blinded study making interpretation difficult. Dr. Eder summarized this complex literature by concluding there is no clear evidence suggesting any biologic agent is superior for enthesitis, and treatment selection should be guided by activity in other domains, response to prior treatment, and patient preference.
Finally, Dr. Eder discussed the entity of vedolizumab-induced enthesitis. Vedolizumab is a gut-specific integrin antagonist that is effective treatment for inflammatory bowel disease (IBD). 12% of patients on this therapy were noted to have new-onset enthesitis, mostly unilateral disease with or without oligoarthritis and dactylitis. This may represent drug-induced disease, or reflect unmasking of disease after discontinuing prior IBD therapy (usually TNF inhibitors). In this cohort, most responded to NSAIDs or local steroid injection, but 27% required change in therapy.
Enthesitis is a key component of the pathophysiology of PsA and axSpA which begins early in the disease process, contributes to disease burden, and portends more aggressive disease. Physical examination is difficult due to the reliance of non-specific tenderness, but can be aided with ultrasound or other imaging modalities. NSAIDs and local steroids can be used with caution, but advanced therapies are effective in the treatment of enthesitis. Further research, however, is needed to best guide therapy between biologic agents for the management of enthesitis.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.