Dermatomyositis Reviewed Save

Researchers from the University of Pennsylvania have published an open-access review of dermatomyositis (DM) - its manifestations, hallmark cutaneous features, etiopathogenesis and treatment options.
DM presents a heterogeneous spectrum of both skin and muscle findings, that is also plagued by poor outcomes and complications such as interstitial lung disease (ILD) and malignancy. Significant advances in myositis-specific autoantibodies, type I interferons, and cytokine dysregulation have improved our understanding DM. This review discusses anti-Mi-2, anti-TIF1γ, and anti-MDA5 subtypes of DM, their diagnosis, prognosis, and treatment strategies.
While glucocorticoids and antimalarials are used in many, many others may have refractory disease, including chronic skin disease. Emerging targeted therapies, including Janus kinase inhibitors and monoclonal antibodies, show promise in addressing type I interferon-driven pathways and refractory symptoms. Future research aims to refine diagnostic criteria, integrate biomarkers, utilize more robust outcome measures, and develop targeted therapeutics to improve outcomes while minimizing treatment-related toxicity. This review consolidates current knowledge and highlights the need for a multidisciplinary, individualized approach to managing DM, focusing on both established and novel treatment avenues.
Highlights from this review include:
- 5 Subtypes of DM
- Classic DM with both characteristic skin findings and muscle inflammation.
- Heliotrope rash (violaceous rash around the eyes)
- Gottron's papules (erythematous papules over knuckles)
- Gottron’s sign (flat erythema over bony prominences, including knuckles but also extending to other areas like elbows and knees.)
- Symmetrical proximal muscle weakness
- Elevated muscle enzymes (creatine kinase, aldolase)
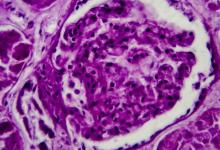
- Abnormal electromyography (EMG), MRI and muscle biopsy
- Clinically amyopathic dermatomyositis (CADM): dermatomyositis sine myositis, with cutaneous features but no muscle involvement
- CADM patients may still have systemic disease, including ILD
- Juvenile Dermatomyositis (JDM): like adult DM but often includes additional systemic involvement. They may be at risk for:
- Calcinosis
- Gastrointestinal vasculopathy
- Lipodystrophy risk
- Dermatomyositis associated with malignancy - often diagnosed around the same time as DM or shortly thereafter.
- Tend to be older age and male gender with certain cancers; Lung cancer is the most prevalent type of cancer in men with DM; Breast and gynecological cancers are the most prevalent types of cancer in women with DM.
- anti-TIF1γ (anti-p155/140) and anti-NXP2 antibodies are implicated in increased malignancy risk.
- Overlap syndromes; when DM coexists with other connective tissue diseases
- Classic DM with both characteristic skin findings and muscle inflammation.
- Underlying causes and mechanisms
- Largley unclear but there are roles for genetic susceptibility, environmental triggers, immune dysregulation exemplified by myositis-specific autoantibodies (MSAs) and evidence suggests the utility of MSAs in diagnosis, prognosis and treatment approaches
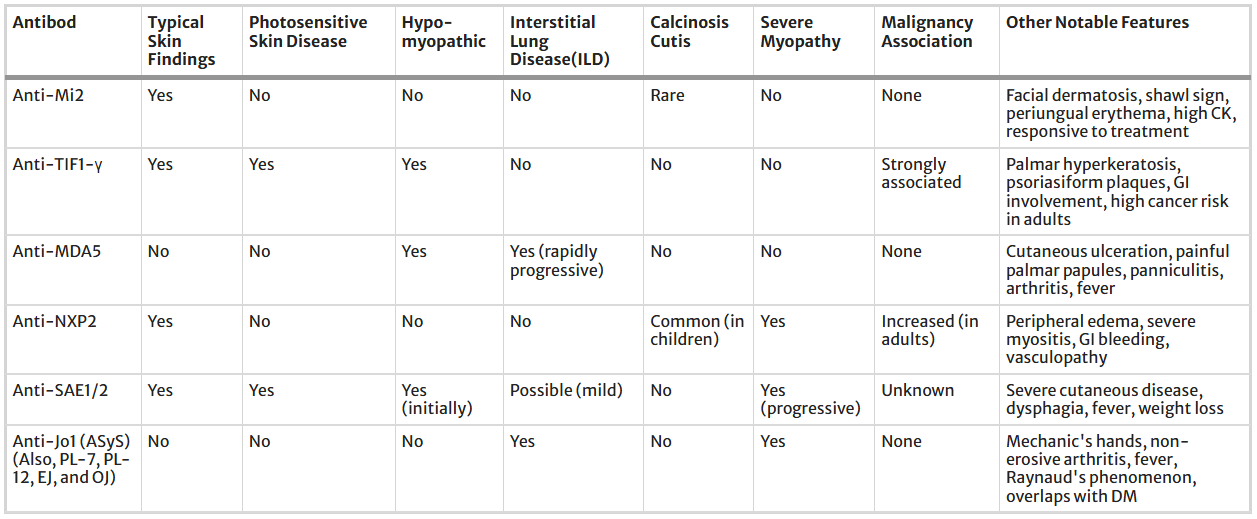
- MSA's have specific clinical phenotypes and may be linked to malignancy risk, ILD, and severe cutaneous involvement
- DM is linked to considerable morbidity and mortality
- Autoantibodies Reviews (MSAs, MAAs,
You can read the full article here - for more information on etiology, pathogenesis, cytokines, genetics, environmental factors, and specific treatment for specific scenarios.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.