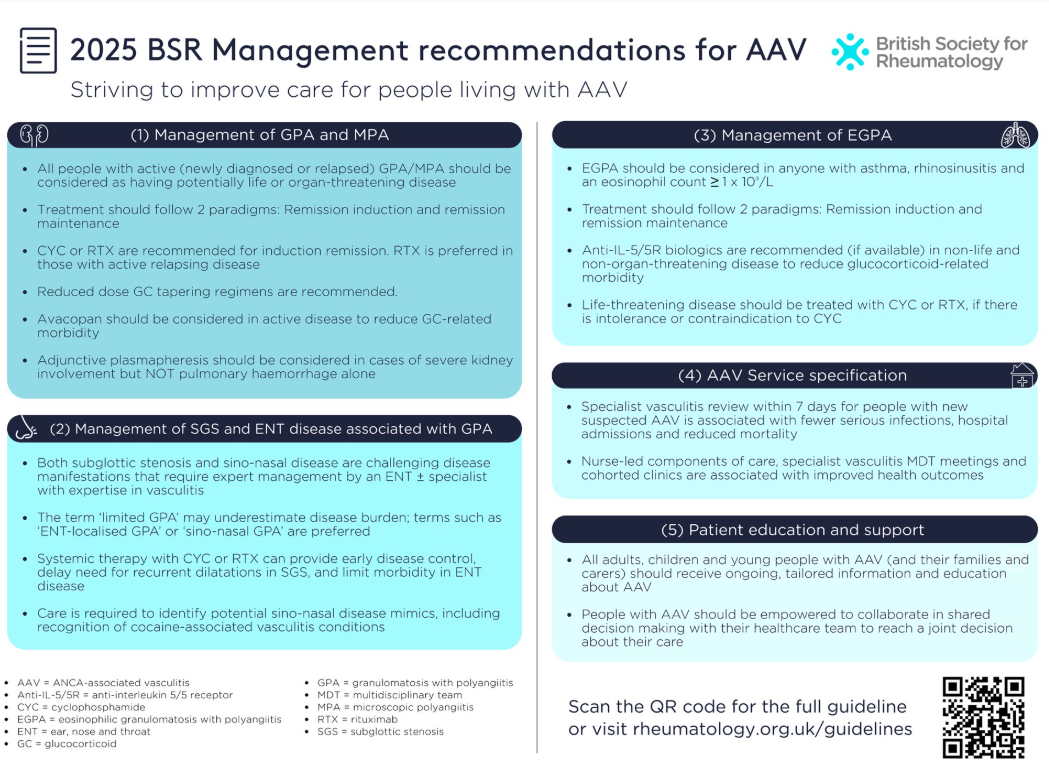
2025 BSR Recommendations for ANCA-associated Vasculitis Save
The British Society for Rheumatology (BSR) and British Health Professionals in Rheumatology (BHPR) have published a guideline for the management of adults with ANCA-associated vasculitis (AAV); specifically three conditions: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA).
In 2021 the American College of Rheumatology and Vasculitis Foundation published their guidelines for the management of Antineutrophil Cytoplasmic Antibody-Associated Vasculitis, Giant Cell Arteritis and Takayasu Arteritis and Kawasaki Disease. This update from the BSR is their first since their guideline for management of AAV was published in 2014.
Thhis updated is prompted by numerous randomized controlled trials, research and recommendations on the management of AAV. These 26 recommendations encompassed five key domains: 1. Treatment for GPA and MPA; 2. Management of subglottic stenosis and ear, nose and throat (ENT) manifestations of AAV; 3. Management and treatment for EGPA; 4. Service specifications; 5. Patient education and support. The BSR working group included mostly rheumatologists but also research nurses, ENT surgeons, nephrologists and trainees.
The evidence was graded using the GRADE approach, as either strong (A), moderate (B) or weak (C). Strength of recommendation were either strong or weak.
Recommendations:
- All people with lived experience of active (newly diagnosed or relapsed) AAV should be considered as having potentially life- or organ-threatening disease (GRADE 1C, SoA 98%)
- GPA or MPA
- All people with lived experience of active GPA or MPA should be assessed for induction of remission treatment with immunosuppressants combined with glucocorticoids (GC) or avacopan (GRADE 1A, SoA 99%).
- The recommended options for immunosuppression for remission induction of newly diagnosed GPA or MPA are intravenous pulsed cyclophosphamide (CYC) or rituximab (RTX) (GRADE 1A, SoA 98%).
- For active relapsing disease, treatment with RTX is preferred (GRADE 1B, SoA 97%).
- A combination of both CYC and RTX can be considered for organ-threatening or life-threatening disease
- \Certain individuals with active GPA or MPA, with no evidence of life- or organ-threatening disease, may be considered for alternative induction therapy with methotrexate (MTX) or mycophenolate mofetil (MMF) (GRADE 1A, SoA 96%).
- Plasmapheresis for GPA and MPA
- Active GPA or MPA and severe kidney involvement with creatinine >300 μmol/l should be considered for adjunctive plasmapheresis provided their risk of potential adverse events has been considered
- For children living with active GPA or MPA, there is insufficient data to routinely recommend plasmapheresis for severe renal involvement; this therefore should only be considered on a case-by-case basis after discussion with an expert centre
- Adjunctive plasmapheresis is not routinely recommended for pulmonary haemorrhage without severe kidney involvement
- Glucocorticoid treatment for GPA and MPA
- In organ- or life-threatening disease, we advocate treatment with oral GC at a starting dose of 50–75 mg or 1.0 mg/kg/day (dependent on weight with a maximum of 75 mg daily). Oral GC (prednisolone) should be tapered in accordance with the PEXIVAS tapering schedule, achieving a dose of 5 mg prednisolone equivalent per day by 4–5 months
- In non-organ- or non-life-threatening disease, lower GC-tapering regimens can be considered, at a starting dose of 0.5 mg/kg/day oral GC (prednisolone), with tapering in accordance with the LoVAS regimen
- Whilst children were not included in PEXIVAS, this tapering regimen can be considered for adolescents. For younger children, the SHARE guideline for prednisolone tapering could also be considered [32]
- Despite commonplace use, there is a lack of supporting trial evidence for intravenous methylprednisolone (IV MP) pulses. Therefore, IV MP pulses are not routinely recommended but can be reserved as an option for the management of organ-threatening manifestations, including active renal disease and diffuse alveolar haemorrhage (GRADE 2C, SoA 97%).
- Avacopan -Patients with active GPA or MPA should be considered for avacopan use as a steroid sparing agent, with or without a short course of glucocorticoids (tapering over four weeks)
- Maintenance of remission treatment for GPA and MPA
- Following induction of remission with an RTX or CYC-based treatment regimen, we recommend maintenance of remission with RTX in preference to other agents
- Maintenance rituximab should be administered at a dosing range of 500 mg to 1000 mg every 4–6 months
- Azathioprine (AZA) or MTX may be considered as alternative options
- MMF is an option only where there is intolerance, or a contraindication, to RTX, AZA or MTX
- GPA and MPA: duration of immunosuppression
- Maintenance of remission should be continued for a period of 24–48 months
- People living with severe renal involvement who remain dialysis dependent have a high risk of infection. Patients with renal limited disease who remain dialysis dependent may not require ongoing immunotherapy. Maintenance of remission therapy to prevent relapse should be balanced against the risks of immunosuppression
- GPA and MPA: duration of GC treatment - The optimum length of treatment with GC during the maintenance phase is uncertain. Depending on concurrent immunosuppression, complete GC withdrawal may be possible within 6–12 months following induction of remission treatment
- Kidney transplant - People living with GPA or MPA should be in stable clinical remission for at least 6–12 months prior to receiving a kidney transplant
- GPA-related subglottic stenosis- Airway symptoms (exertional dyspnoea, stridor) associated with GPA should be investigated by an Ear, Nose and Throat (ENT) and/or Respiratory specialist with expertise in vasculitis and airway stenosis
- Treatment of subglottic stenosis - GC therapy can help reduce inflammation in GPA-sub-glottic stenosis but is not the preferred option for maintenance therapy. More significant disease requires induction and maintenance therapy following the recommendations for systemic GPA and MPA treatment
- Sino-nasal GPA - ‘limited GPA’ may underestimate disease burden; terms such as ENT-localised or sino-nasal GPA are preferred
- Integrated multi-disciplinary assessment in sino-nasal GPA - All people living with AAV affecting the sino-nasal tract should be offered multi-disciplinary assessment that includes input from ENT surgeons and physicians experienced in the management of AAV
- Cocaine-associated vasculitis conditions - History of previous and current cocaine use should be assessed (both drug history and toxicology) at baseline in all individuals suspected of having AAV and repeat toxicology screening considered in patients with persistent or refractory sino-nasal disease
- Treatment for sino-nasal disease
- Immunosuppression: first line treatment with RTX or CYC and GC or avacopan for organ-threatening ENT disease is recommended as this provides early disease control and limits accrual of damage
- Topical and local symptomatic treatments should be offered to people living with sino-nasal disease
- Screening for bacterial carriage and infection, and antimicrobial treatment where indicated, should be offered to people living with sino-nasal disease
- Sino-nasal reconstructive surgery - It is essential that disease is in remission for at least 12 months (and desirable that maintenance prednisolone dose is ≤5 mg) at time of reconstructive surgery, otherwise high failure and complication rates are frequently observed
- EGPA management - A diagnosis of EGPA should be considered in any individual with a combination of asthma (especially of adult-onset), chronic rhinosinusitis (with or without nasal polyposis) and peripheral eosinophilia typically ≥1 × 109/L who develop end-organ involvement
- Dx of EGPA - The diagnosis of EGPA can be challenging due to the heterogeneous clinical phenotype and requires a specialized multi-disciplinary approach to exclude alternative eosinophilic syndromes – MDT discussion and consensus are encouraged when ratifying the diagnosis of EGPA
- Management of EGPA should be stratified according to clinical manifestations and disease severity
- Induction of remission for EGPA
- All people living with active (newly diagnosed or relapsed) EGPA should be considered as having potentially life- or organ-threatening disease
- All people living with active EGPA should be assessed for induction of remission treatment with GC combined with other immunomodulatory agents
- The recommended immunomodulatory options for people with life- or organ-threatening EGPA are intravenous pulse CYC as first line OR RTX if CYC is either contraindicated or not acceptable to the patient
- Anti-IL-5/IL-5R directed therapies (both ligand and receptor) have demonstrated broad efficacy in EGPA and are recommended (if available for any of the licensed indications) for remission induction in non-life or non-organ-threatening disease
- In non-life- or organ-threatening active EGPA, alternative induction therapy with MTX, MMF or AZA may be considered when anti-IL-5/IL-5R is not available or as adjunctive therapy depending on disease phenotype
- Maintenance of remission for EGPA
- Anti-IL-5/IL-5R directed therapies are recommended (if available for any of the licensed indications) for maintenance of remission and to aid tapering of GC
- RTX, MTX, MMF or AZA may be considered as alternative options when anti-IL-5/IL-5R is not available, or as adjunctive maintenance therapies depending on disease phenotype
- GC should be tapered to the lowest possible effective dose whilst maintaining disease remission and considering patient-specific disease manifestations, comorbidities and preferences
The manuscript provides additional recommendations for Integrated care, timely services, specialist centres, patient education, shared decision making and future research.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.