Paradoxical Reactions, Target Selection & the Future of Imaging in Psoriatic Care Save
“It’s Not the Same Psoriasis”: Understanding Paradoxical Reactions
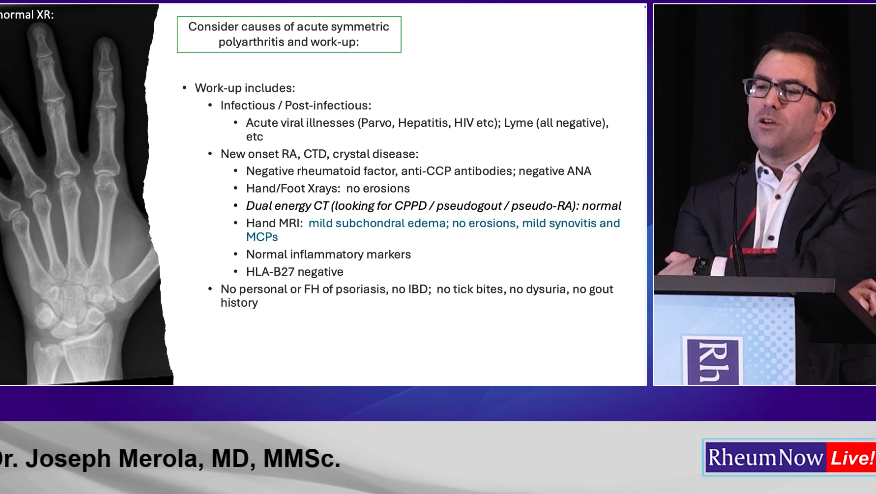
At RheumNow Live, Dr. Joseph Merola from UT Southwestern presented a compelling discussion on paradoxical immune reactions in psoriatic disease. He began with a case of a 60-year-old woman with mild psoriasis who, after 17 months on a TNF inhibitor, developed palmoplantar pustular disease with deep-seated pustules.
“This is not a flare of her old psoriasis,” he emphasized. “It’s a morphologic shift — and it’s likely TNF-induced.”
TNF inhibitor–induced psoriasis is most strongly associated with infliximab and occurs more commonly in women. It may arise de novo or represent a phenotype change in patients with psoriatic arthritis. Histopathology reveals a mixed psoriasiform and spongiotic dermatitis — described as “a bridge between eczema and psoriasis.” Biopsy studies demonstrate increased type I interferon signaling in paradoxical lesions, with elevated MxA expression compared to classical psoriasis.
Management strategies include topical therapies and phototherapy for mild disease, with methotrexate or JAK inhibitors considered for more resistant cases. Dr. Merola noted that treatment does not always require immediate discontinuation of TNF therapy but should reflect understanding of the immune axis involved.
Paradoxical reactions also occur with IL-17 inhibitors, where approximately 6% of patients develop an atopic dermatitis–like phenotype, often in those with a personal or family history of atopy. Conversely, dupilumab has been associated with inflammatory arthritis, reported in observational cohorts with symptom onset weeks to months after initiation and present with diffuse/symmetric joint pain. In general, the arthritis resolved after cessation of dupilumab but may last for weeks-months following. Dr. Merola suggests appropriate work up to rule out other cases. For mild disease, consider treating through. For moderate disease, consider NSAIDs, low dose prednisone, combo approach such as adding MTX or holding dupilumab and or switching to other mechanism. For severe disease, consider steroid taper, addition of DMARD, hold dupilumab or consider oral JAK.
IL-17 vs IL-23: Speed, Durability, and Domain Coverage
The second major theme focused on cytokine selection in psoriatic disease. Rather than declaring a superior class, Dr. Andre Rbeiro MD emphasized domain-based treatment selection tailored to individual patient profiles.
Head-to-head trials provide nuance. The ECLIPSE trial demonstrated that guselkumab (IL-23) achieved superior PASI 90 responses at week 48 compared with secukinumab (IL-17), although IL-17 inhibitors showed faster early responses. Similarly, IXORA-R highlighted rapid early skin clearance with ixekizumab, with convergence of outcomes over time.
In psoriatic arthritis, trials such as SPIRIT-P1/P2 (ixekizumab) and DISCOVER-1/2 (guselkumab) demonstrated robust ACR responses in TNF-inadequate responders. Axial disease remains an area of investigation, with IL-17 inhibitors having established efficacy and emerging data evaluating IL-23 blockade.
Comorbidities influence choice. Data support IL-23 efficacy in inflammatory bowel disease, often favoring this class in patients with Crohn’s disease. Shared decision-making, safety, pregnancy planning, cardiometabolic risk, and patient preference remain critical components of therapy selection.
On the horizon are the next wave of targeted therapies currently being studied, including sonelokimab (IL-17A/F inhibitor) and icotrokinra (oral IL-23 inhibitor), as well as exciting new head-to-head trials. The BE BOLD trial compared bimekizumab vs risankizumab with a primary endpoint of ACR50 response at wk16. The IZAR-2 trial is exploring sonelokinmab vs risankizumab. These trials will provide crucial data to refine treatment strategies and help clinicians make even more evidence based decisions.
From Sharp Scores to Artificial Intelligence: Imaging's Next Chapter
The final presentation by Dr. Arthur Kavanaugh MD addressed the evolution of imaging in rheumatology. The Sharp score, developed by Dr. John Sharp and colleagues, became a cornerstone for evaluating structural damage.
The ATTRACT study demonstrated that TNF inhibitors significantly reduced radiographic progression in rheumatoid arthritis, reshaping expectations for long-term structural preservation.
Ultrasound and MRI now offer earlier detection of synovitis and erosions. Emerging modalities such as PET imaging and high-resolution peripheral quantitative CT (HR-pQCT) may provide molecular and microstructural insight, including differentiation of true bone repair from imaging artifact.
Automation and artificial intelligence–enhanced ultrasound systems promise standardization and efficiency in clinical practice. As therapies advance, imaging tools must evolve to match the precision of modern immunologic treatment.
Across paradoxical reactions, cytokine selection, and imaging innovation, the central message is clear: psoriatic disease management now requires precision across immune pathways, clinical domains, and outcome measurement.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.