SpA: Etiology to Diagnosis to Treatment - An Abstract Roundup Save
This year’s ACR Convergence was a great success especially given its unique circumstances. There were a lot of interesting abstracts and presentations on spondyloarthritis (SpA) encompassing a wide range of topics from etiology to diagnosis to treatment.
First let’s focus on a hot topic for many of our rheumatologic diseases, which is the gut microbiome. We are beginning to see distinct gut microbiome populations and diversity in our diseases including spondyoarthritis. We are seeing gut microbiome differences in ankylosing spondyloarthritis (AS) compared to inflammatory bowel disease and healthy patients (Abs#1310). We’re also seeing some differences in gut microbiome in sub-groups of patients with axial spondyloarthritis based on disease activity and duration, enthesitis, and radiographic involvement (Abs#1853).
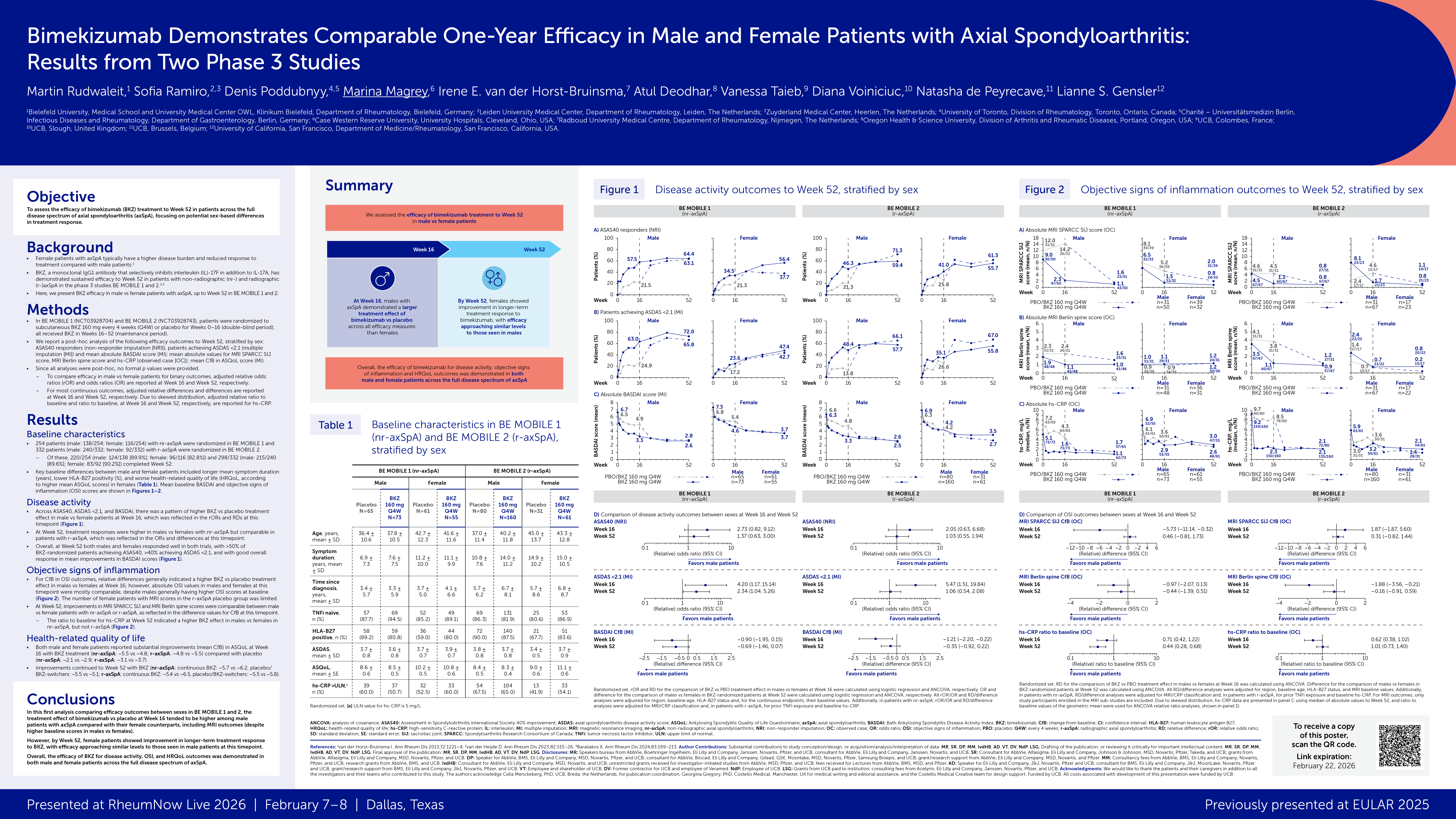
Gender disparities were another focus in our patients with SpA. In patients with AS, women had more achilles tendonitis, plantar fasciitis, joint swelling, BASDAI>40 and more DMARD use (Abs#1872). Another study showed that in patients with axial SpA, women were older at onset, had longer symptom duration and more peripheral joint pain and lower frequency of HLA-B27 (Abs#0876). Lastly, a very important subject for our female patients is pregnancy. A large study of 4 prospect cohorts in Europe studied pregnancy outcomes in women with AxSpA and found favorable outcomes overall. There were 3% with pre-eclampsia, 6-9% with gestational diabetes, and 0-5% with preterm birth (Abs#1498). The pre-term birth rate was similar to WHO reported rates of 9% in Europe.
As far as treatment, there were many abstracts on known treatments for psoriatic arthritis and SpA such as filgotinib, guselkumab and tildrakizumab showing consistent efficacy through 52 weeks. There was a late-breaking abstract on a phase 2b, 16 week, double-blinded, placebo controlled, randomized controlled trial on the TYK2 inhibitor, deucravacitinib for treatment of psoriatic arthritis. This study showed improved ACR20/50/70 responses compared to placebo, improved HAQ-DI response, enthesitis resolution, and MDA versus placebo. Lastly there were no serious adverse effects reported (Abs#L03). It will be interesting to see what phase 3 studies show in the future.
In the context of imaging and diagnosis of SpA there were a few studies focusing on the use of musculoskeletal ultrasound (US) especially in relation to enthesitis. One study found an improvement in US enthesitis scores at 6 months, which correlated with biologic initiation or change and overall clinical improvement (Abs#1552). There was also a study correlating clinical findings with US findings of the synovial-entheses junction (Abs#0311). US was also a good tool in differentiating our PsA patients with concurrent fibromyalgia as US scores did not correlate with higher clinical scores in these patients (Abs#0315).
Lastly, with the continued emergence of machine learning and artificial intelligence, there continues to be ongoing research on the implementation of these tools, especially in diagnosis. There was an artificial intelligence model which was validated to detect radiographic sacroiliitis (Abs#2018) and machine learning identified 9 signatures including nail psoriasis, CRP and 7 biomarkers to distinguish PsA from psoriasis patients without arthritis (Abs#0502).
Many of these abstracts are pragmatic and useful in our everyday practice as we continue to treat patients with SpA and some of these abstracts are more theoretical and may take more time before we see the fruits of their labor. However, it would be not surprising to see a day, in the not so distant future, where a patient answers a questionnaire from a computer and with the help of artificial intelligence, labs, biomarkers and imaging are analyzed and the latest biologic is then prescribed.
The question then will be, what is the role of the rheumatologist in that scenario?
Editor's note: This article was originally published November 10, 2020, and is being shared again this week.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.