All News
Hydroxychloroquine's World of Confusion - What you Need to Know
Hydroxychloroquine has been a dominant news item since the start of the COVID-19 crisis, with a great deal of misconceptions by those who don't know or use or take the drug. HCQ leaped to the headlines on March 19th when President Trump endorsed the drug as being “approved” by FDA. Of course at that time, it was still only approved for SLE, RA and malaria and it wasn't until 2 weeks later (March 31st) that the FDA issued an "emergency use authorization" allowing the use of either chloroquine or HCQ for treatment of severe, hospitalized patients with COVID-19.
To provide clarity and evidence - here are some of the facts you need to know.
Hydroxychloroquine and QTc Prolongation
JAMA Cardiology reports the risk of QT (QTc) prolongation when hydroxychloroquine (HCQ) was given to hospitalized patients with coronavirus disease 2019 (COVID-19), especially when given with azithromycin.
Read ArticleRare Inflammatory Syndrome in Kids with COVID-19
Pediatricians are asking the question - could this be a rare manifestation of COVID-19 in children?
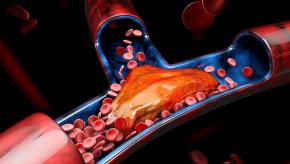
Read ArticleTNF Inhibitors Reduce and Stabilize Coronary Plaque
Arthritis & Rheumatology reports that biologic (bDMARD) use in rheumatoid arthritis may decrease cardiovascular disease risk by retarding coronary plaque formation and progression (especially non‐calcified and low‐attenuation plaque).
Read ArticleHigh Dose Chloroquine Harmful in Severe COVID-19
JAMA Open Network reports an interim analysis of the Brazilian CloroCovid-19 trial showing thta higher doses of chloroquine (CQ) in the treatment of severe COVID-19 was associated with QTc interval prolongation and increased mortality.
Read ArticleRheumNow Podcast – In Times of Trouble (4.24.20)
Dr Jack Cush reviews the news, journal reports, twitter feed and COVID developments from the past week on RheumNow.com
Read ArticlePotential Role of B Cells in COVID
A pre-proof letter to the editor in the Journal of Allergy and Clinical Immunology presents a series of patients with immunoglobulin deficiency disorders and how they differentially responded when infected with the coronavirus.
They identified seven Primary Antibody Deficiencies patients with COVID-19 infection; five affected with Common Variable Immune Deficiencies and two affected with Agammaglobulinemia, one with X-linked Agammaglobulinemia and one with Autosomal Recessive Agammaglobulinemia.
NIH Consensus Guidelines for the Treatment of COVID-19
A National Institutes of Health (NIH) expert panel has developed consensus treatment guidelines for the management of coronavirus (COVID-19). To date no drug has been proven to be safe and effective for treating COVID-19. Moreover, they found no evidence to recommended the use of hydroxychloroquine for prophylaxis or treatment of COVID-19 outside of a current clinical trial.
Read ArticleCOVID-19 Systemic Involvement
The presentations of the COVID-19 infection have been clearly chronicled with the worrisome onset of sore throat, dry cough, loss of smell and taste with fevers, myalgias, fatigue and the worrisome progression of pulmonary involvement in a minority. Lab findings may include a leukocytosis,
Read ArticlePost 9/11 Autoimmune Disease Risk
The 9/11/01 terrorist attach on the World Trade Center (WTC) resulted in at least 2,977 fatalities, over 25,000 injuries, and caused at least $10 billion in infrastructure and property damage. Arthritis & Rheumatology reports that dust cloud exposure among responders and
Read ArticleNICE Guidelines on Managing Rheumatologic Conditions During COVID-19 Pandemic
On April 3rd, the National Institute for Health and Care Excellence (NICE) in the UK, published a rapid guideline for managing children and adults with rheumatological autoimmune, inflammatory and metabolic bone disorders during the COVID-19 pandemic, while protecting staff from infection.
Read ArticleDr. Artie Kavanaugh - Don't Stop!
Drs. Cush and Kavanaugh discuss the downside of stopping hydroxychloroquine, DMARDs and biologics in lupus, RA and pregnancy.
Read ArticleCOVID-19 Rheumatology News
With the COVID-19 pandemic dynamically changing, we have provided several news items germane to the Rheumatologist.
Read ArticleIn Lupus, Keep BP Below 130/80
Blood pressure should be maintained at a level below 130/80 mm Hg in all patients with lupus to lessen their likelihood of atherosclerotic vascular events, Canadian researchers asserted.
Read ArticleRheumNow Podcast- Corona Increases RA Risk (3.13.20)
Dr. Jack Cush reviews the news and journal articles from the past week on RheumNow.com.
Read ArticleEMA Final Recommendations on VTE Risk with Tofacitinib
On 14 November 2019 the European Medicines Agency (EMA) concluded that Xeljanz (tofacitinib) could increase the risk of blood clots in the lungs and in deep veins in patients who are already at high risk. These recommendations have been formally published and are intended for EU nation
Read ArticleRheumNow Podcast - Despite Corona (3.6.20)
Dr. Jack Cush reviews the news and journal articles from the past week on RheumNow.com.
Airway Inflammation Drives Rheumatoid Risk
A cohort analysis of the Nurses' Health Study suggests that asthma and COPD are associated with increased risk for incident rheumatoid arthritis (RA), independent of smoking- thus airway inflammation may be an important factor in the evolution of pre-cllnical RA.
Read ArticleFolate Levels Protect from CV Mortality in RA
In a study of rheumatoid arthritis (RA) patients, JAMA reports that serum folate level of greater than 4.3 ng/mL was associated with lower CV mortality risk.
Read ArticleRheumNow Podcast- Methotrexate Mechanisms (2.28.20)
Dr Jack Cush Reviews the news and journal articles from the past week on RheumNow.com
Read Article