Best of 2022: The Enthesitis Challenge in Psoriatic Arthritis Save
Editor's note: this blog originally published on April 6, 2022, and is being shared again as a Best of 2022. Enjoy!
A colleague of mine once told me an interesting story of how her father, who was a doctor, misdiagnosed his wife with fibromyalgia when she actually had psoriatic arthritis with enthesitis all along. I would venture out and say that the average physician would have trouble evaluating enthesitis because even we, as rheumatologists do!
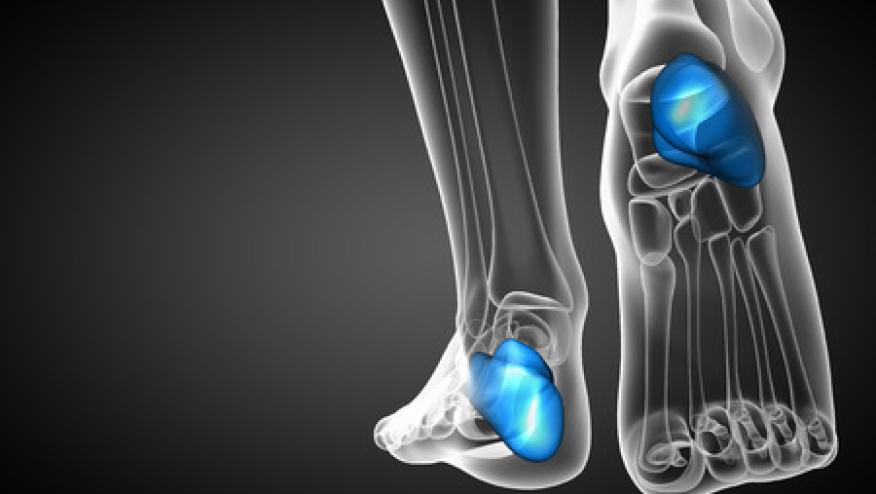
Enthesitis is the inflammation of enthesis, which is the connective tissue between tendons or ligaments and bone. We have over 100 entheses in our bodies, which by the sheer quantity alone would make examining for enthesitis difficult. The Achilles tendon is the classic enthesis most of us are familiar with, but after that, how do we choose which entheses to examine next?
Although complex, we do know that enthesitis is prevalent in psoriatic arthritis patients with systematic reviews showing enthesitis to be present in 30% of psoriatic arthritis patients.
What is the best way to examine for enthesitis? Do we stick with the tried-and-true method of the doctor poking at a site of pain and if the patient says “ow,” they’ve now been diagnosed with enthesitis? How accurate is that, especially for the smaller enthesis sites? There are numerous clinical trial standardized methods for quantitative enthesitis assessments (MASES, SPARCC and Leiden enthesitis index) – but their complexity and lack of uniformity obviates their use as a practice tool. Luckily, imaging modalities have improved and can aid us in diagnosis.
Magnetic resonance imaging (MRI) can certainly assist in the enthesitis evaluation, but there are questions regarding how pragmatic that approach may be. Is it possible to order an MRI every time the patient potentially has enthesitis pain? It is also important to keep in mind that by the time a patient’s MRI is approved, then scheduled, there is a good chance the original site of pain may have migrated.
Musculoskeletal ultrasound is another tool that can provide the rheumatologist with real time imaging evaluation for enthesitis. New ultrasound scoring systems are standardizing how the rheumatologist assesses for enthesitis in psoriatic arthritis patients. There have also been studies showing ultrasound improvement of enthesitis after biologic treatment. However, musculoskeletal ultrasound is certainly not standard of care amongst all rheumatologists and the results can certainly be operator dependent. Nevertheless, ultrasound is practically useful in differentiating psoriatic arthritis enthesitis from fibromyalgia tender point pain as there is anatomical overlap in pain sites in these disorders. If a patient has pain close to or at an enthesis site without imaging evidence of enthesitis, would that then be fibromyalgia? An unanswered and harder question is what if the ultrasound shows inflammation, but the patient does not have pain.
In terms of treating enthesitis, there is no clear best choice. The good news is we have treatments that can help treat enthesitis, but we do not know yet which one works best. We know biologic therapies that inhibit TNF, IL-17, IL-12/23, IL-23, JAK and PDE4 all have comparable efficacy in PsA enthesitis, but we lack robust head-to-head trials to differentiate between these. We have also seen studies show a dramatic response in the treatment of mild to moderate enthesitis but not so much for severe enthesitis. This aspect of psoriatic arthritis treatment will undoubtedly need more of a precision medicine approach in the future as we tailor individual treatment plans based on a patient’s predominant disease phenotype.
I challenge each rheumatologist to consider how they evaluate for and manage enthesitis. How do you examine for enthesitis or better yet, what (or how many) sites do you choose to examine? Is it time to expand to more sites? Should we use imaging modalities like ultrasound more often to differentiate psoriatic arthritis patients with enthesitis from those with fibromyalgia and vice versa? Lastly, are you going to change how you treat an enthesitis predominant psoriatic arthritis patient?
Join The Discussion
As you say, enthesitis a common cause of pain in PsA, but Fibromyalgia is present in up to 20% of patients with PsA, better clinical exam does help, simple palpation at points of tenderness is not advisable, pain on resistance at entheseal insertions more sensitive. Elbow, wrist, hand, knee and ankles are easily accessible. New US machines with high frequency probes 18-24MhZ are proving more useful in defining tendon morphology and improved Doppler such as SMI may also help. Big problems remain assessing tendons in patients who are older, have a history of physical work and repetitive injuries and assessing tendons in the feet and ankle in patients with high BMI. GRAPPA are working on it and we await results from their studies. The enthesitis indices must be revised to a more useful clinical set - studies are needed to see which sites will reveal the best clinical outcome and be measurable in clinical studies. Current studies mention the enthesitis indices often as a secondary outcome measure and this is unfortunately the best measure we have at the moment but far from ideal.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.