Large Vessel Vasculitis: Giant Cell Arteritis and Takayasu Arteritis Save
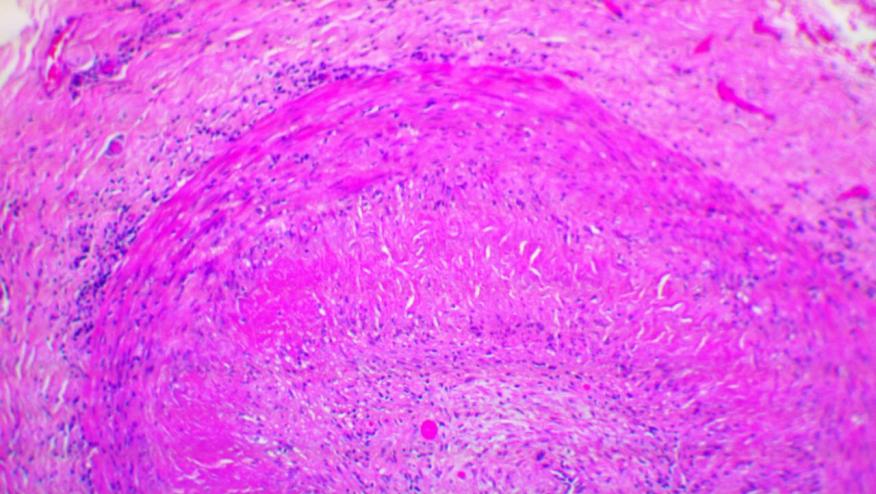
Prof Weyland started by explaining that giant cell arteritis (GCA) and Takayasu Arteritis (TA) are granulomatous forms of arteritis. The age of onset is usually >60 years in GCA and < 40 years in TA, the group in the middle may be a different form of vasculitis based on gene expression studies.
GCA can be split into a vascular and an extra-vascular component. The vascular component affects the aorta and is driven by T cell immunity. The extra-vascular component is primarily PMR and is driven by a hepatic acute phase response.
Then Dr Kermani reviewed diagnosis and management of GCA. She noted that physical examination has poor sensitivity for diagnosis (14-50%). It is important to remember that imaging studies have suggested 50% prevalence of thoracic aorta involvement at diagnosis. Data also suggests an increased risk of stroke and venous thromboembolic disease in the first year of diagnosis, the predominate type of stroke is the vertebrobasilar stroke.
Prompt treatment starts with 40-60mg of glucocorticoids with the aim to prevent visual loss. Pulse steroids in those patients with visual loss at presentation is often utilised. The routine use of aspirin is not recommended however unless they require this medication for their cardiovascular disease. The data on the efficacy of methotrexate is conflicting but a meta-analysis has suggested a reduced risk of relapse and a reduction in the total steroid dose. Unfortunately, anti-TNF therapy does not show benefit.
Tocilizumab at 8mg/kg versus placebo showed good efficacy in GiACTA trial, this therapy is now an FDA approved therapy for GCA. Abatacept has also been studied in GCA in a phase II trial, more patients in the treatment group had relapse free survival compared to placebo (48% abatacept vs 31% placebo). A phase III study of abatacept for GCA is underway.
Then Dr Grayson discussed imaging of GCA. The diagnostic value of ultrasound in GCA from several trials shows varying sensitivity of 10-68% and specificity of 81-100%. So, most notably the sensitivity is widely variable. The Tabul study only found a 70% agreement between ultrasound and temporal artery biopsy (Luqmani et al, 2016).
FDG-PET may be able to see vessel inflammation but has drawbacks including the interference with steroids and diabetes, as well as the radiation exposure. Notably there are issues with specificity because in comparator diseases like atherosclerosis 17% will have a FDG-PET reported as showing active vasculitis in the NIH PET cohort. The take home message is not to make the diagnosis of GCA solely on the imaging findings.
Angiography with MR and CT are non-invasive and can be used but specificity of the images also can be a problem. For all modalities there can be considerable variability in how images are interpreted so this presents a major limitation in the use of imaging to diagnose GCA.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.