ICYMI: Reduction of AxSpa-Associated Acute Anterior Uveitis with Certolizumab Save
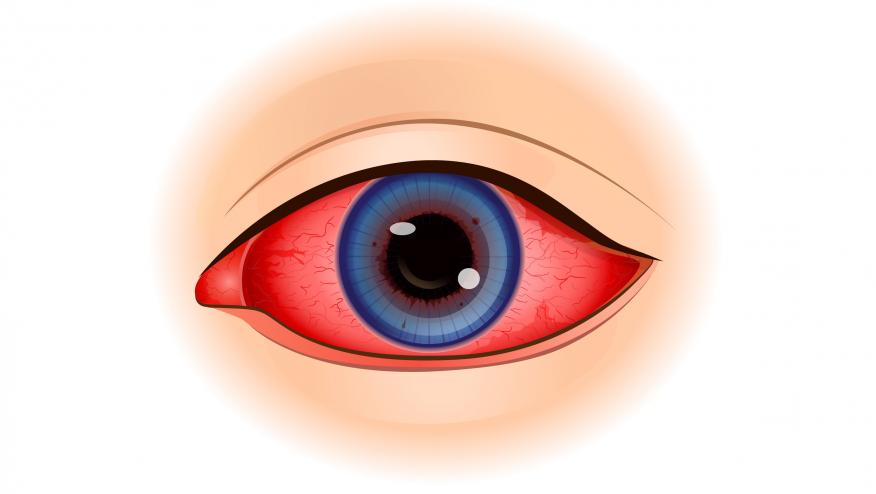
Acute anterior uveitis (AAU) is the most common extra-musculoskeletal manifestation in axial spondyloarthritis (axSpA), affecting up to 50% of patients in some age groups. AAU can have a significant impact on quality of life with risk of permanent visual deficits if not adequately treated.
As a review, the VISUAL trials assessed adalimumab (ADA) efficacy in the treatment of uveitis; STOP-Uveitis showed improvement with tocilizumab (TCZ); and the FAST trial compared methotrexate (MTX) and mycophenolate (MMF) in uveitis.
- VISUAL I by Jaffe et al in 2016 (NEJM) showed a 50% decrease (HR 0.5, p = 0.001) in risk for inflammation recurrence when taking adalimumab compared to placebo in 217 patients with active non-infectious intermediate, posterior, and panuveitis. The median time to treatment failure was 24 weeks in ADA and 13 weeks in the placebo (PBO) group.
- VISUAL II by Nguyen et al in 2016 (Lancet) showed that the median time to treatment failure > 18 months in the ADA arm versus 8.3 months in the placebo arm (HR 0.57, p = 0.004) in 226 patients with inactive non-infectious intermediate, posteriors, or pan-uveitis controlled by 10-35 mg/day of prednisone
- STOP-Uveitis by Sepah et al in 2017 (Am J Ophthalmol)
- showed improvement in vision, reduced vitreous haze, and decreased macular edema at 6 months with TCZ in 37 patients with non-infectious intermediate, posterior, or panuveitis.
- VISUAL III by Suhler et al in 2018 (Ophthalmology) showed 242 active uveitis patients who received ADA were likely to achieve quiescence, improve visual acuity, and reduced daily uveitis-related systemic steroid use. Most patients (129 of 371) with inactive uveitis at study entry sustained quiescence without a systemic steroid dose increase.
- FAST trial by Rathinam et al (JAMA) in 2019 was a randomized controlled trial that compared oral MTX 25 mg weekly vs MMF 1.5 g twice daily with standardized prednisone taper in 216 patients with noninfectious intermediate, posterior and pan-uveitis. The primary outcome was treatment success at 6 months showing MTX noninferior to MMF (66.7% MTX vs 57.1% MMF, p = 0.2). Further research is needed to determine if either drug is more effective based on anatomical subtype of uveitis.
The first study to prospectively investigate certolizumab pegol (CZP) in AAU patients with active axSpA at high risk of recurrent AAU was the C-VIEW study by Van Der Horst-Bruinsma et al that was published in 2021. The C-VIEW study showed that CZP treatment significantly reduced AAU flare rate in patients with axSpA and history of AAU indicating that CZP is a suitable treatment option for patients at risk for recurrent AAU. Of note, CZP was FDA-approved in 2013 for ankylosing spondylitis and in 2019 for non-radiographic axSpA but not yet approved for AAU.
The C-VIEW study in 2021 (link) was a 104-week (96 weeks, plus 8 week safety follow-up), open label, multicenter study that included patients with active axSpA, HLAB27 positivity, and a history of recurrent AAU (≥ 2 AAU flares in total; ⩾1 in the year prior to baseline) . Of 115 enrolled patients, 89 initiated CZP with 83 completing week 96. Patient characteristics were 63% male, 85% had radiographic axSpA, 15% had non-radiographic axSpA, and mean disease duration ~9 years). There was a significant 82% reduction in AAU flare event rate during CZP versus pre-baseline. One hundred percent and 59.6% of patients experienced ≥1 and ≥2 AAU flares pre-baseline, respectively, compared to 20.2% and 11.2% during treatment.
Abstract 0524 presented at the 2023 American College of Rheumatology Convergence conference in San Diego, California compared patients from the C-VIEW study with matched high-risk axSpA patients from the University of California San Francisco (UCSF) and University Health Network Toronto Western Hospital (UHN) who were receiving non-biologic standard care. More specifically, 89 patients who received CZP in the C-VIEW study were compared to 66 bio-naïve patients (40 from UCSF, 26 from UHN). Conventional synthetic DMARD use was similar between groups at baseline and follow-up. After adjustment for confounders were made, the AAU flare rate was significantly lower with CZP that in the matched comparator population with an 87% reduction in AAU flare rate (p<0.0001) associated with CZP treatment. There were no statistically significant differences in mean BASDAI and distribution of ASDAS disease activity states at baseline between the CXP-treated and comparator groups. Overall, CZP is a promising therapeutic option in managing recurrent AAU flares.








If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.