IL-23 Targeting for Enthesitis in Psoriatic Arthritis Save
Treatment with guselkumab (Tremfya) was effective in resolving enthesitis among patients with psoriatic arthritis (PsA), a post-hoc analysis of two phase III trials found.
At week 24, 45% of patients receiving subcutaneous guselkumab every 4 weeks and 50% of those given the medication every 8 weeks had resolution of enthesitis compared with 29% of those randomized to placebo (P=0.0301 for both), according to Dennis McGonagle, MD, PhD, of the University of Leeds in England, and colleagues.
Rates of enthesitis resolution continued to rise, reaching 58% of all guselkumab-treated patients by week 52, the investigators reported online in Rheumatology.
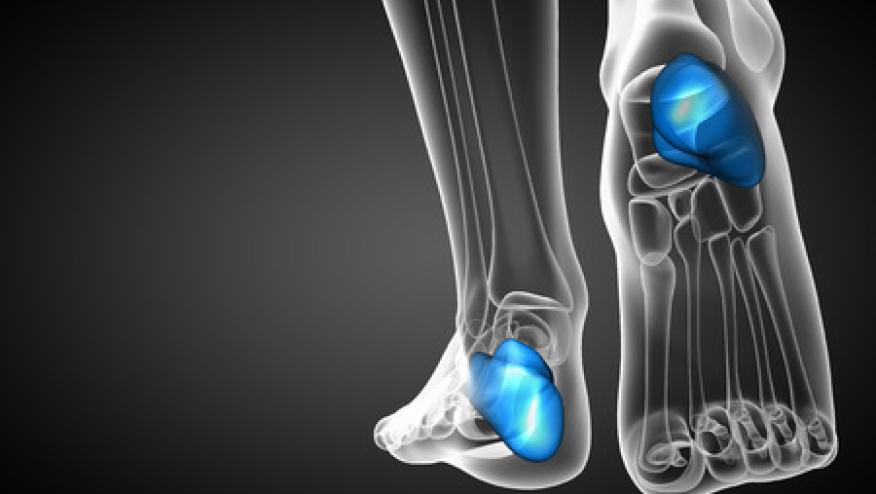
Enthesitis -- inflammation at the site of tendon, ligament, or joint capsule insertion into bone -- is an important component of PsA affecting more than half of patients. "As a potential antecedent to inflammatory and structural changes in the joint and a predominant source of pain, enthesitis confers greater disease burden in patients with PsA. Resolution of enthesitis is associated with improvements in function, health-related quality of life, and pain," they wrote.
The interleukin (IL)-23/IL-17 axis has been implicated in the pathogenesis of PsA overall and in enthesitis specifically. Guselkumab is an anti-IL-23 p19 subunit monoclonal antibody that is licensed for use in psoriasis and PsA. Multiple aspects of PsA demonstrated benefits with guselkumab in two pivotal clinical trials, DISCOVER-1 and DISCOVER-2.
DISCOVER-1 enrolled 381 patients who could have previously taken one or more tumor necrosis factor inhibitors, while DISCOVER-2 included 739 patients who were biologic-naive. In both studies, patients continued standard treatments, including oral glucocorticoids, nonsteroidal anti-inflammatory drugs, and conventional disease-modifying antirheumatic drugs such as methotrexate or hydroxychloroquine.
In the primary analysis of these two studies, significant differences compared with placebo were observed for multiple efficacy endpoints. "We further analyzed the pooled DISCOVER-1 and DISCOVER-2 data, to comprehensively investigate the efficacy of guselkumab in both resolving and preventing enthesitis," McGonagle and colleagues wrote.
Patients were randomized to receive subcutaneous guselkumab, 100 mg every 4 weeks or every 8 weeks, or placebo. After week 24, patients initially assigned to receive placebo were given guselkumab 100 mg every 4 weeks.
Enthesitis was measured on the Leeds Enthesitis Index, documenting the presence of painful entheses at the lateral epicondyle humerus, the medial femoral condyle, and the Achilles tendon insertions. Enthesitis was defined as mild if the enthesitis index score was 1, moderate if the score was 2, and severe if scores were 3 or higher.
At baseline, 65% of patients in the two studies had enthesitis, with mean enthesitis index scores of 2.8. Those who experienced enthesitis more often were women, those with a body mass index of 30 or higher, and those with a mean Global Assessment of Psoriasis score of 4 and a Psoriasis Area and Severity Index of 20 or higher, as well as other features suggesting more active disease such as severe dactylitis and higher swollen and tender joint counts.
Median time to resolution of enthesitis was 16 weeks in both guselkumab groups compared with 24 weeks in the placebo group.
At week 24, the Cohen d values for change in the enthesitis index from baseline were 1.07 and 0.91 in the every-4-weeks and every-8-weeks groups, respectively, which represented a large effect size.
In patients with mild enthesitis, resolution by week 24 was observed in 68% and 66% of the every-4-weeks and every-8-weeks groups, respectively. By week 52, resolution was seen in 70% to 75% of patients overall, including 80% of the patients initially assigned to placebo who crossed over to guselkumab at week 24.
Among patients with moderate enthesitis, resolution was seen by week 52 in two-thirds, but fewer than half of patients with severe enthesitis achieved resolution by week 52. Patients with severe enthesitis more often were women, had long disease duration, and also typically had a higher body mass index, potentially implicating mechanical factors that may not be responsive to biologic therapy, the authors pointed out.
When the investigators considered enthesitis resolution and clinical responses in other disease manifestations, they found that at weeks 24 and 52, patients with resolution of enthesitis also were more likely to have minimal disease activity, normal scores for disability, and swollen/tender joint counts of 1 or less.
No new-onset enthesitis was reported by up to 87% of patients at week 52, including among patients who crossed over from placebo. "While this suggests that guselkumab may inhibit the development of enthesitis, it may also be due to inherent patient and disease differences between those with and without enthesitis," the authors noted.
A limitation of this analysis was the lack of an active comparator in the DISCOVER trials. "It will be important to further investigate whether targeting the IL-23 p19 subunit is superior to inhibition of tumor necrosis factor and IL-17 in treating PsA patients with enthesitis," they concluded.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.