Osteoporosis Screening in High-Risk Men Save
A Veterans Affairs (VA) Health Systems study of older male veterans found benefits of a remote model of screening that significantly improved osteoporosis screening, treatment, and adherence compared with usual care, with high patient and clinician acceptance.
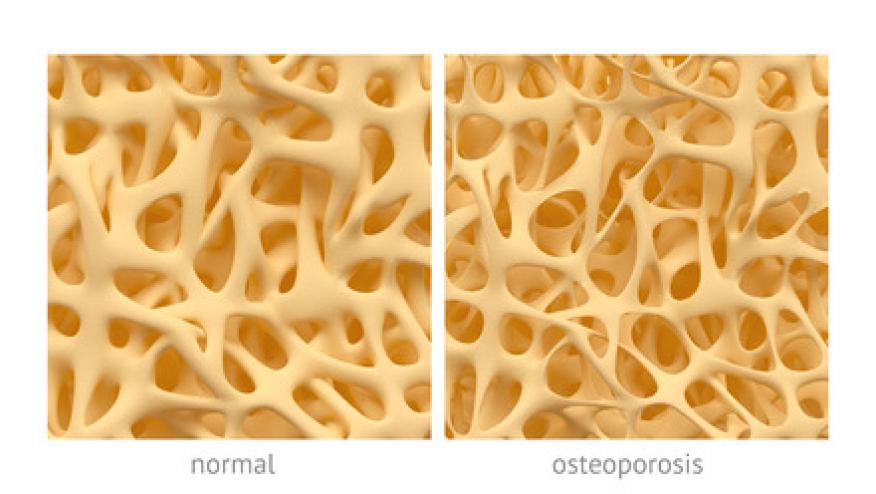
There is limited evidence supporting osteoporosis screening in men, especially in primary care.
This study tested the impact of a centralized, remote bone health service (BHS) on screening, treatment, adherence, and bone density in older men with fracture risk factors. The randomized clinical trial involved 39 primary care teams in 2 Veterans Affairs (VA) Health Systems that included 3112 male veterans aged 65 to 85 years who had at least 1 fracture risk factor but had no prior fractures.
BHS screening included dual-energy x-ray absorptiometry (DXA) scan, followed by an electronic consult to their primary care clinician, nurse care manager and PCP team.
Participants were older (mean 73.3 years); mostly black [40%] or white [56%]; with half (49%) of the BHS group screened vs 2.3% of the usual care group (P < .001). More than half of those screened (51%) had osteopenia or osteoporosis.
Over 84% of the BHS group initiated osteoporosis treatment and achieved high levels of adherence and high persistence to OP therapies over 2 years of follow-up. There was less mean femoral neck T-score change over 2 years in the BHS vs usual care groups (−0.55 vs −0.70, P = .04).
Facilitation of bone screening in high risk men (BHS model) resulted in significantly better outcomes compared with usual care, with a higher average femoral neck bone density at 2 years. The approach of using fracture risk factors to select men for screening yields a comparable proportion of men diagnosed with osteopenia or osteoporosis with screening of women 65 years or older.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.