RA-ILD in the Spotlight at ACR 2024 Save
Over the past 5 years, there has been growing interest in RA-ILD due to its relative prevalence and severity. This seems to be one of the few RA outcomes not improving much, even with the advent of expanded treatment options. There is also a shocking lack of trial data. Despite this being the most common systemic rheumatic diseases, only three trials have enrolled a total of 217 patients to treat ILD. Thus, the recently published 2023 ACR/CHEST treatment guideline recommendations were all conditional based on low quality evidence.
This year, there were two oral sessions dedicated to RA-ILD, one of which even the overflow room was standing room only, in addition to many posters. These collectively spanned the entire disease course of RA-ILD.
RA-ILD risk factors
Studies from the Veteran’s Administration, led by Dr. Bryant England, continue to inform RA-ILD risk and outcomes, since it is enriched with ILD due to predominance of men and smoking. This year, several abstracts investigated the combined effect of clinical factors, genetics, and circulating biomarkers for RA-ILD. The highlight was abstract #799 that included 5 genetic factors and 63 biomarkers that were able to accurately find RA-ILD cases. Next steps will be to replicate in another population and to identify a simple model that could be implemented clinically. Abstract #1905 used similar data to risk stratify people at very high or very low RA-ILD risk using the MUC5B promoter variant and two circulating biomarkers.
There has been a debate on how RA factors may impact ILD risk. Our group, led by Dr. Gregory McDermott, found that an RA genetic risk score (GRS) had no association with ILD using data from the Mass General Brigham Biobank in abstract #800. However, the RA GRS worked well to predict RA, seropositive RA, and earlier age at RA onset.
Screening for RA-ILD
We presented the baseline results of the multi-center SAIL-RA study that is enrolling patients with new-onset RA to investigate lung health. In abstract #802, Dr. McDermott presented results of the first 172 patients. The prevalence of ILD in early RA was 11%, and 16% had any parenchymal lung disease. We found strong associations with moderate/high disease activity (OR 7) as well as RA onset at age 60 or older and male sex. We then applied other RA-ILD screening strategies as external validation in early RA. These included ANCHOR-RA, ACR/CHEST guideline, ESPOIR, and the Four Factor Score. Even with simple clinical data, these all performed well (AUC ~0.80). If using the SAIL-RA factors of older age, male sex, and moderate/high disease activity, the number needed to screen was only 3.6 if people had at least 2 of these factors (sensitivity 0.79; specificity 0.73). Thus, we are getting closer to being able to screen for RA-ILD, but we still need to understand whether early detection may modify outcomes.
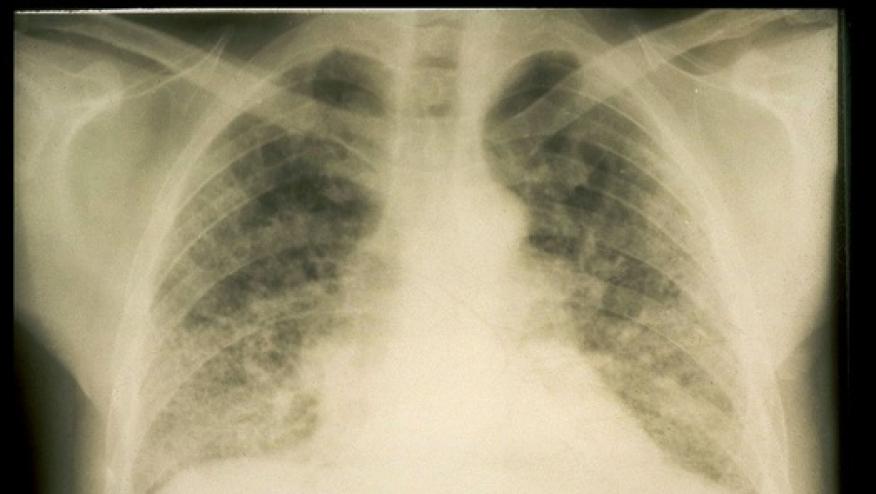
Another highlight on screening was abstract #2222. This used a strategy of assessing symptoms, auscultation, plain chest x-ray, and DLCO to monitor pulmonary involvement. Any abnormality would then prompt chest HRCT. Unlike many prior studies, this had lengthy follow-up (mean 10.2 years). During follow-up, 21% developed ILD and 43% developed any parenchymal lung disease, even without all patients receiving HRCT.
Progression of RA-ILD
Most previous RA-ILD studies have investigated mortality for progression. In collaboration with the nationwide Korean KORAIL study, our group applied the recent definition for progressive pulmonary fibrosis by ATS/ERS/JRS/ALAT to RA-ILD. This definition uses symptoms, chest HRCT features, and pulmonary function tests. Abstract #2234, presented by Dr. Sung Hae Chang, developed a risk model for RA-ILD progression. Overall, 35% had ILD progression, and risk factors included usual interstitial pneumonia CT pattern, high extent of ILD, low DLCO, high-titer anti-CCP, RA disease activity, and pulmonary damage biomarkers such as KL-6 and hSP-D. Interestingly, no inflammatory markers were associated with RA-ILD progression. A model incorporating these factors worked well to risk stratify. The model could help prioritize more intense monitoring or treatment with medications such as antifibrotics.
Treatment of RA-ILD
Of course, treatments are what we really need to improve outcomes in RA-ILD. It has remained unclear how DMARDs for RA may help or hurt ILD. Abstract #1713 presented by Dr. Frideres is the most comprehensive analysis on b/tsDMARDs and RA-ILD treatment. This used VA data to perform an emulated target trial. Despite rituximab being recommended as first-line treatment in the recent ACR/CHEST guideline, there was no difference in risk of death or respiratory hospitalization comparing abatacept, IL-6 inhibitors, and JAK inhibitors. It is unclear whether this is due to low power or confounding, or perhaps these drugs equally treat or harm our patients.
In conclusion, we have made significant progress in defining the risk factors, who to screen, who will progress, and how to treat RA-ILD. There is still a dearth of knowledge. Trials are urgently needed to evaluate screening and treatment strategies for RA-ILD










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.