Whole Body MRI for Arthritis Save

Whole-body MRI (wbMRI) reviews have increasingly appeared in the medical literature, owing to better scanners, faster imaging times and reduced costs. Used of such non-oncologic musculoskeletal imaging provides high-contrast resolution images of the entire body or selected regions screening, diagnosis, staging, and surveillance purposes.
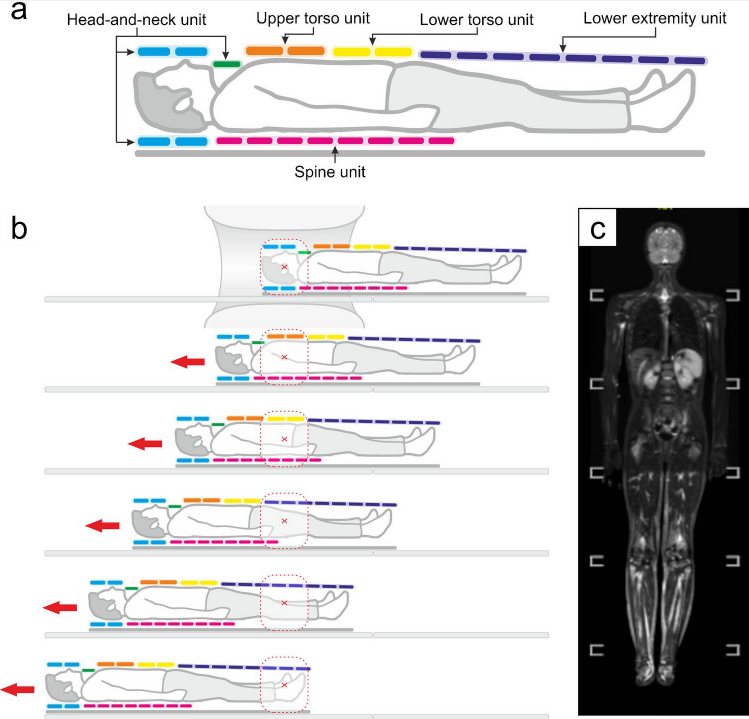
Whole-body MRI refers to a series of contiguous vertex-to-toes coronal images acquired sequentially across multiple “stations” of 25–50 cm each and stitched together post-imaging. Total wbMRI scan time ranges between 45 and 75 minutes plus a setup time of 5–10 minutes. This can be truncated with narrower coverage (e.g., orbits-to-knees, shoulders-to-hips) to fit the clinical scenario.
wbMRI may be beneficial in identifying inflammatory arthritis (eg, RA, SpA, JIA, osteitis, etc) - all characterized by multifocal involvement of both skeletal and extra-skeletal sites.
The advantage of wbMRI includes the detection of subclinical disease foci, quantitative assessment of the total disease burden, greater detail (especially for intraosseous and axial involvement) and the lack of ionizing radiation.
Compared to plain radiography, conventional ultrasound, and targeted MRI, wbMRI offers better sensitivity and reproducibility. makes it ideal for monitoring autoimmune diseases also in sensitive cohorts.
Further research is needed to validate scanning protocols, cost-effectiveness, and utility in routine clinical practice.
A comprehensive, full-read review is available here.
Another prospective imaging study, used gadolinium contrast-enhanced whole-body MRI, to evaluate patients receiving immune checkpoint inhibitors (ICI) who developed arthritis; 35 [58%] with arthralgia and 25 [42%] with inflammatory arthritis) and 20 healthy controls were recruited. Three distinct inflammatory patterns were seen: peripheral inflammatory arthritis in 22 (37%) of 60 patients; polymyalgia rheumatica in seven (12%), and an overlapping phenotype of polymyalgia rheumatica and peripheral inflammatory arthritis in 12 (20%). MRI abnormalities were commonly detected (joint synovitis, joint erosions, enthesitis, tenosynovitis) in ICI patients with arthralgia or inflammatory arthritis, more than that detected by exam alone.
Join The Discussion
Hi Jack,
I understand your skepticism, but I do think it adds substantially to the evaluation of some new patients and also D2Ts and have been excited about this for a while. Most Rheumatologists of the older generation felt very strongly about their trust on physical exam. Although it is a fantastic skill we hone daily, it is still an imperfect and limited one. Ultrasound evaluation has been shown to change diagnosis in many new patients evaluated for polyarthralgia which was not felt to be inflammatory on exam. It is possible that over time those patients would have declared themselves more clearly and there is a risk of overdiagnosis with more sensitive tools, I would acknowledge that. However, I think this expands the possibilities of early diagnosis of inflammatory arthritis and possibly more effective management or even prevention of development into classic, "full blown", phenotypes. I agree that we need further studies before deploying this in clinical practice to better understand what patient population, if any, this would be appropriate.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.