Earlier treatment with biologics to reduce the risk of organ damage in systemic lupus erythematosus (SLE) Save
- SLE disease activity and treatment-associated toxicities can lead to organ damage in approximately 30–50% of patients within 5 years.2–4
In an Italian inception cohort, 22% of 230 patients with early SLE (within 12 months of SLE classification) had organ damage after one year of follow-up.1
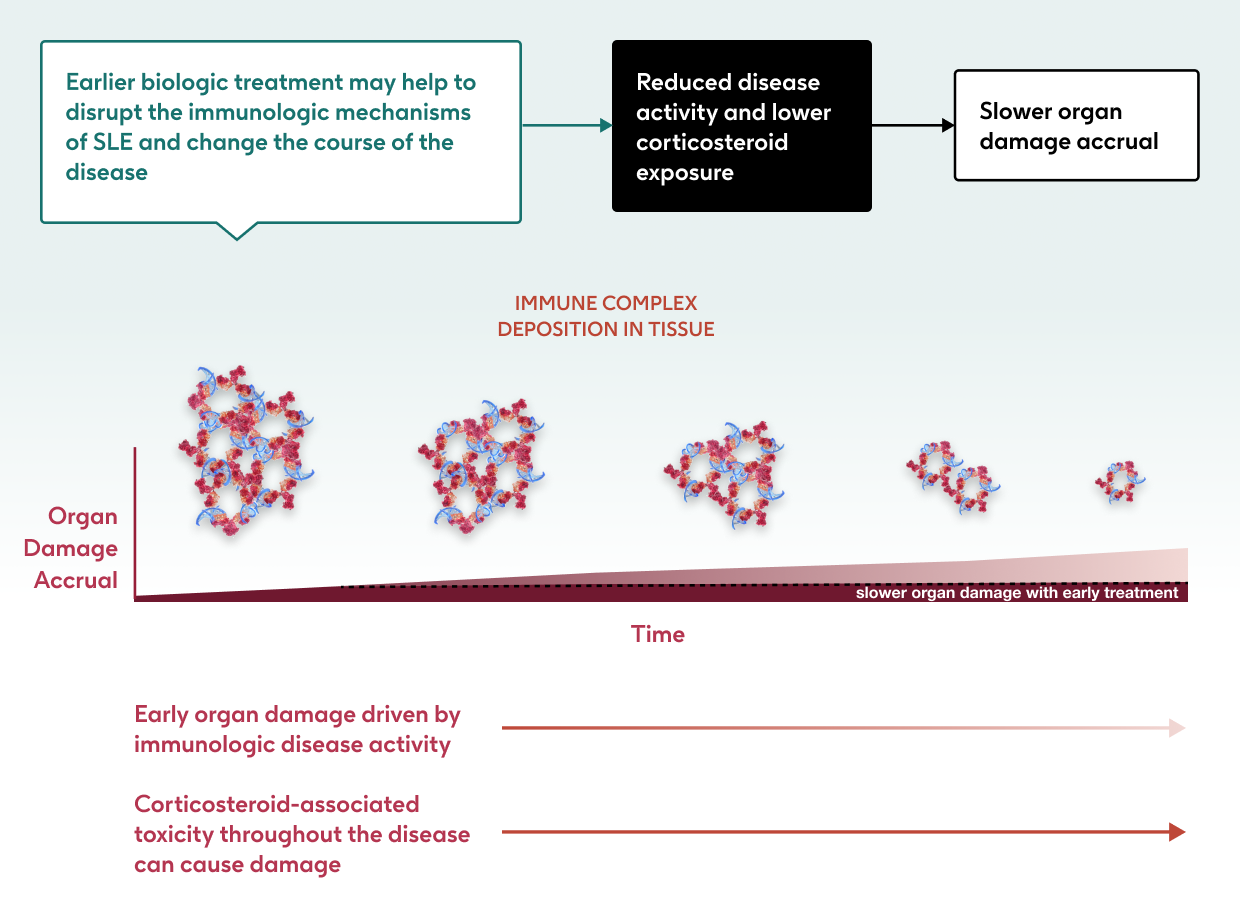
Optimizing treatment as early as possible may help to reduce risk of organ damage.5
Understanding the complex pathophysiology of SLE may help us to specifically address the underlying mechanisms of disease with treatment.6,7
Click below to watch our 4-minute SLE pathophysiology animation and learn more about the underlying mechanisms of the disease.
Why should we aim to optimize treatment earlier in SLE?
Many patients may not receive effective treatment quickly enough after SLE diagnosis.
- One UK study of 802 patients reported an average delay of >5 months from diagnosis to treatment, during which time patients may have experienced flares (median [95% confidence interval] time to flare: 63 [57, 71] days).8
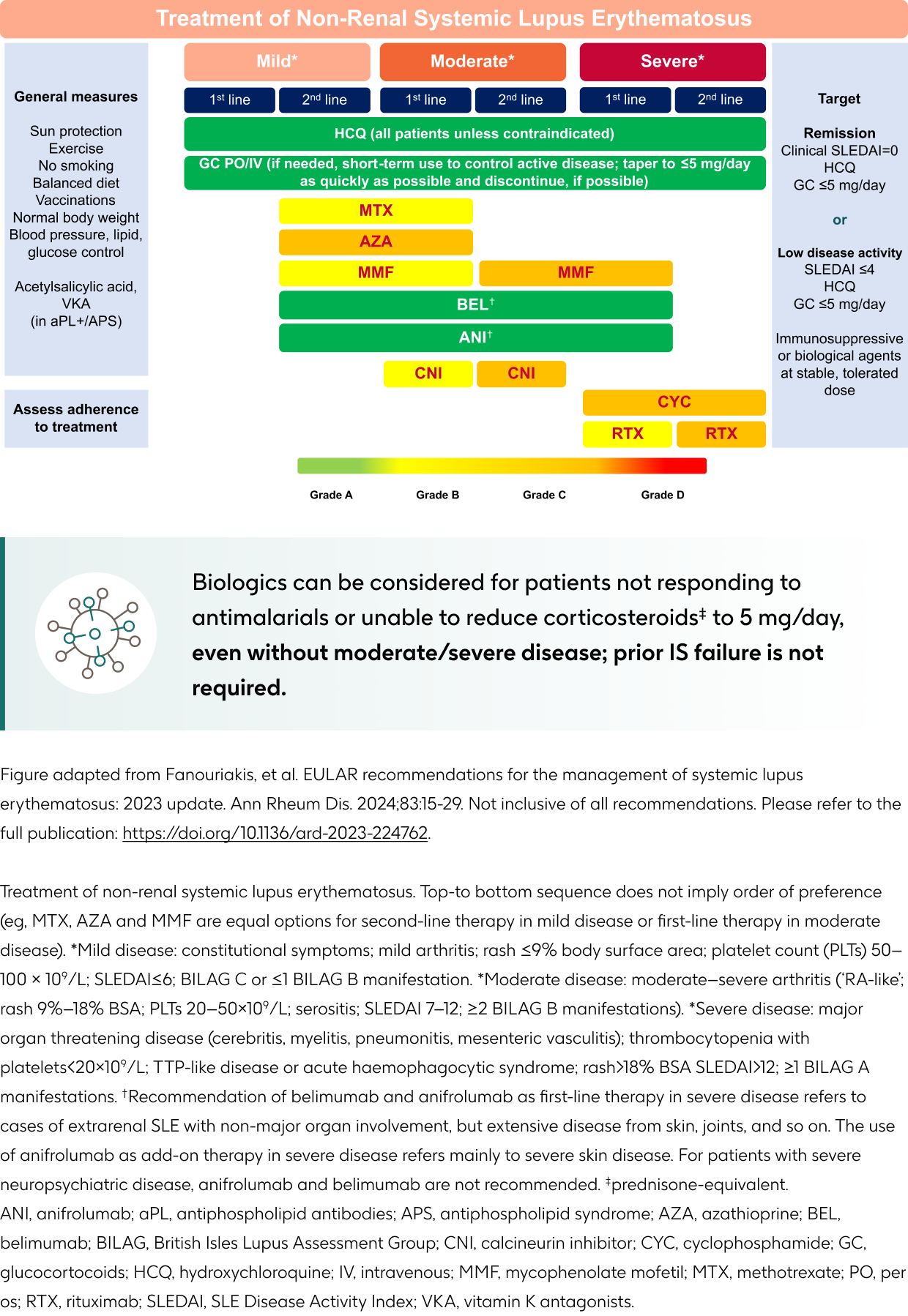
- The 2023 EULAR recommendations for the management of SLE emphasize early intervention, with treatments aiming at remission or low disease activity state to prevent organ damage and improve a patient's prognosis.9
Early effective treatment and early disease control can slow organ damage and improve patient outcomes.10-13
- In an inception cohort of patients with new onset SLE and a mean follow-up of four years – those who did not achieve early disease quiescence in Year 1 had increased disease activity, steroid use and organ damage during follow-up compared with those with early quiescence:11

Due to their detrimental effects, the 2023 EULAR recommendations state that corticosteroids should ideally only be used as a bridging therapy, and tapered to ≤5 mg/day prednisone-equivalent, or withdrawn when possible.9
What are the 2023 EULAR recommendations regarding biologics in SLE?
- Changing the course of SLE disease early may help to slow the accrual of damage and attain treatment targets - patients with lower accrued damage are the most likely to reach remission.15
- This approach is reflected in the 2023 EULAR recommendations for SLE, which state that biologics can be used to control disease activity and reduce corticosteroid exposure without mandatory prior use of a conventional immunosuppressant, including in patients who have not responded to antimalarials or those unable to reduce corticosteroids to acceptable doses.9
- The 2023 EULAR treatment recommendations summarized below reflect a shift towards the use of biologics earlier in the disease course.9
To learn more about the 2023 EULAR recommendations and what these may mean for your patients, listen to our podcast below presented by Dr. Narender Annapureddy, an Associate Professor of Rheumatology at Vanderbilt University Medical Center.
What other strategies may help us to minimize risks of organ damage in SLE?
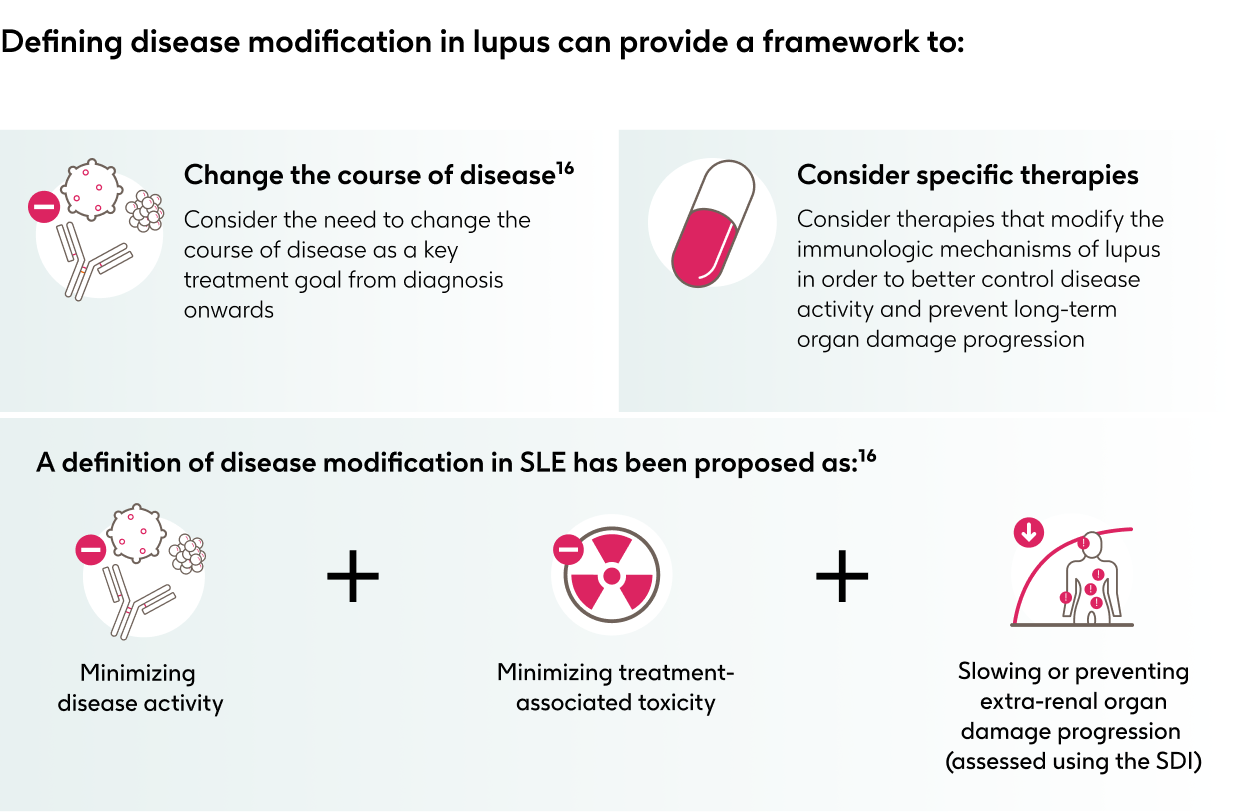
Modifying the course of disease by targeting the underlying pathophysiological mechanisms is a key treatment goal in many chronic diseases, and disease modification is a known concept in numerous therapeutic areas.16
PSE-US-2970 | August 2024
- Piga M, Floris A, Sebastiani GD, et al. Risk factors of damage in early diagnosed systemic lupus erythematosus: results of the Italian multicentre Early Lupus Project inception cohort. Rheumatology (Oxford) 2020;59:2272-81. https://doi.org/10.1093/rheumatology/kez584.
- Chambers SA, Allen E, Rahman A, et al. Damage and mortality in a group of British patients with systemic lupus erythematosus followed up for over 10 years. Rheumatology (Oxford) 2009;48:673-5. https://doi.org/10.1093/rheumatology/kep062.
- Stirnadel-Farrant HA, Golam SM, Naisbett-Groet B, et al. Healthcare Resource Use and Costs Associated with Organ Damage in Newly Diagnosed Adults with Systemic Lupus Erythematosus in the UK. Rheumatol Ther 2023;10:1183-97. https://doi.org/10.1007/s40744-023-00567-9.
- Urowitz MB, Gladman DD, Ibañez D, et al. Evolution of disease burden over five years in a multicenter inception systemic lupus erythematosus cohort. Arthritis Care Res (Hoboken) 2012;64:132-7. https://doi.org/10.1002/acr.20648.
- Doria A, Gatto M, Zen M, et al. Optimizing outcome in SLE: treating-to-target and definition of treatment goals. Autoimmun Rev 2014;13:770-7. https://doi.org/10.1016/j.autrev.2014.01.055.
- Allen ME, Rus V, Szeto GL. Leveraging Heterogeneity in Systemic Lupus Erythematosus for New Therapies. Trends Mol Med 2021;27:152-71. https://doi.org/10.1016/j.molmed.2020.09.009.
- Moulton VR, Suarez-Fueyo A, Meidan E, et al. Pathogenesis of Human Systemic Lupus Erythematosus: A Cellular Perspective. Trends Mol Med 2017;23:615-35. https://doi.org/10.1016/j.molmed.2017.05.006.
- Langham J, Barut V, Samnaliev M, et al. Disease severity, flares and treatment patterns in adults with systemic lupus erythematosus in the UK: a real-world observational retrospective cohort analysis. Rheumatol Adv Pract 2021;5:rkab061. https://doi.org/10.1093/rap/rkab061.
- Fanouriakis A, Kostopoulou M, Andersen J, et al. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann Rheum Dis 2024;83:15-29. https://doi.org/10.1136/ard-2023-224762.
- Floris A, Piga M, Perra D, et al. Treatment target in newly diagnosed systemic lupus erythematosus: The association of lupus low disease activity state and remission with lower accrual of early damage. Arthritis Care Res 2020;72:1794-9. https://doi.org/10.1002/acr.24086.
- Nossent J, Kiss E, Rozman B, et al. Disease activity and damage accrual during the early disease course in a multinational inception cohort of patients with systemic lupus erythematosus. Lupus 2010;19:949-56. https://doi.org/10.1177/0961203310366572.
- Piga M, Floris A, Cappellazzo G, et al. Failure to achieve lupus low disease activity state (LLDAS) six months after diagnosis is associated with early damage accrual in Caucasian patients with systemic lupus erythematosus. Arthritis Res Ther 2017;10:19:247. https://doi.org/10.11862Fs13075-017-1451-5.
- Akhavan PS, Su J, Lou W, et al. The early protective effect of hydroxychloroquine on the risk of cumulative damage in patients with systemic lupus erythematosus. J Rheumatol 2013;40:831-41. https://doi.org/10.3899/jrheum.120572.
- Yang B, Zhao M, Wu H, et al. A Comprehensive Review of Biological Agents for Lupus: Beyond Single Target. Front Immunol 2020;11:539797. https://doi.org/10.3389/fimmu.2020.539797.
- Petri M, Magder LS. Comparison of Remission and Lupus Low Disease Activity State in Damage Prevention in a United States Systemic Lupus Erythematosus Cohort. Arthritis Rheumatol 2018;70:1790-95. https://doi.org/10.1002/art.40571.
- van Vollenhoven R, Askanase AD, Bomback AS, et al. Conceptual framework for defining disease modification in systemic lupus erythematosus: a call for formal criteria. Lupus Sci Med 2022;9:e000634. https://doi.org/10.1136/lupus-2021-000634.







