ICD-10: ABCs of the New Code Save
Unless you’ve been living in a cave, you are probably aware that come Oct 1, 2015, the old ICD-9 coding system will be completely replaced with a “newer version”: ICD-10. The purpose of this newer system is to modernize coding,coding; recognizing that since the last update in 1979, the number and precision of diagnoses has increased dramatically. Unfortunately, with only a maximum of 5 characters to use, ICD-9 is currently limited to around 13,000 codes. By expanding this to a maximum of 7 characters, at least 68,000 diagnoses are being considered under ICD-10. Also, the newer coding system will allow for greater specificity and laterality (left/right).
Under the newer system, the first character will always be a letter (alpha character), which will specify the organ system involved. For many, but not all, rheumatologic diagnoses, this will be “M”. The next 2 characters can be either a number or alpha (#2 will always be a number, #3 can be either a number or alpha), and will define a category of diseases. For example, chronic gout: M1A; inflammatory arthropathies: M05-M14; OA: M15-M19; Systemic Connective Tissue Diseases: M30-36; and Spondyloarthropathies: M45-M49.
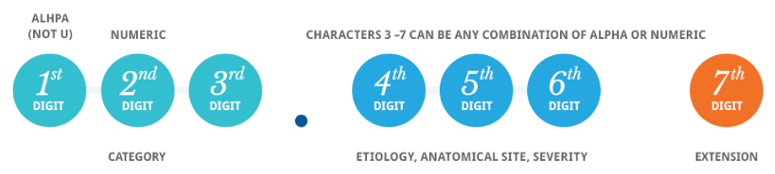
These 3 characters are always followed by “.” (period) before the next characters, if needed, are to be added. Character 4 will describe features like etiology or organ system (RA lung: M05.1, RA other: M05.8....by the way, there is a different code for seroposivite RA (M05) and seronegative RA(M06). Character 5 will be location (wrist=3, knee=6, multiple sites=9) and character 6 will be laterality (right=1, left=2, bilateral=3). The last character will be for additional features, such as tophi (chronic idiopathic gout of the right wrist with tophi=M1A.0911; no tophi=M1A.0910). Confused yet? Wait, there’s more. Sometimes there is no laterality, so a placeholder “X” is added (Chronic idiopathic gout, multiple sites with tophi=M1A.09X1).
Some codes can exist by themselves (Gout: M1A,xxxx, xxxx, seropositive RA: M05.8xxx, PMR: M35.3). Others can be reported as combinations with another disease (IBD related right knee arthritis due to Crohn’s disease=M07.661 and K50.918). Still others need to be reported in combination with other diagnoses, but is a specific order (Reactive Arthritis of the Left ankle due to Yersinia infection=A04.6 (which must be listed first) and M02.172).
My recommendations for implementation of ICD10
The first recommendation I have is to start NOW, if not sooner. Summer is rapidly coming to an end and October will soon be upon us. Once this date happens, anything you code using the old system WILL BE REJECTED!! (Editor’s note: Dr. Bergman’s advice is spot on. Note that CMS and the AMA have stated that they will be “lenient” in the first year of implementation. What that means remains to be seen – JC)
Do you bill using a computer? (Hopefully, a rhetorical question.) Make sure NOW that your software is able to handle ICD10. Using a billing service? Make sure NOW that they are able to handle ICD10.
Buy a coding book. Let’s face it; while there is logic to this system, it is far from intuitive. Having a comprehensive code book, like the ones provided by the AMA (disclosure, I am a member, but not otherwise affiliated) and learn to use it. This is not the time or place to save money. Remember what I wrote above…failure to use these codes will lead to your claims being REJECTED!!
Start small, but get to work. The good news is: for the most part we use the same codes over and over again. We are not FPs who must have every code in the book entered into our computers. More likely we will need 100-200. While that sounds like a large number, it is far from daunting.
I’m starting with the most common codes (RA, Gout, Joint Pain, and Joint Swelling). A list of the most commonly used codes in rheumatology is available on the ACR website: http://www.rheumatology.org/Portals/0/Files/Rheumatology%20ICD-10%20Cros.... (Editor's note: this link was updated on 8/12/15)
Once those are in the system, I’m going through my entire list of frequent codes, A-Z and changing the codes, one at a time. If I do 10-20 per day, which is not unrealistic, I should be through this in under a month.
Educate your staff, especially your billing folks, about the new codes. Did I mention that if you don’t use the new codes, your billing WILL BE REJECTED. Once you have a list of effective codes, re-create your super-bill (if you are still using them) or let your computer system generate the bills, after you have added them.
Anticipate problems and have ready cash available during the transition period. Even in the best of circumstances, problems are bound to occur. This is a nationwide roll-out, glitches are bound to occur. Being ready is always the best option.
If all of this sends you into panic mode, the other option is to pay a service to do this for you. There are many out there who are more than willing to assist you in this transition, for a fee. I’m not making enough in clinical practice to have me want to share it with others, but that is my decision. You may feel differently.
Regardless, the time to act is NOW, if not yesterday. October will be here, soon enough. Do you know where your reimbursements will be?










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.