Impact of glucocorticoids: more than just toxicity Save
As the sole effective treatment for polymyalgia rheumatica (PMR) since their development in the 1950’s until recently, the impact of glucocorticoids and PMR outcomes are undeniably intertwined. So much so that when the OMERACT PMR working group first set out to develop a PMR core outcome set, they quickly realised that many of the outcomes important to patients were related to their glucocorticoid use. Hence the Outcome Measures in Rheumatology (OMERACT) Glucocorticoid Impact working group was established.
Initially named the GC Toxicity working group, patient engagement quickly highlighted that the impact of glucocorticoids is much broader than toxicity alone, and includes treatment benefits as well as harms, with impacts that are important to patients often differing from those deemed most important by clinicians1.
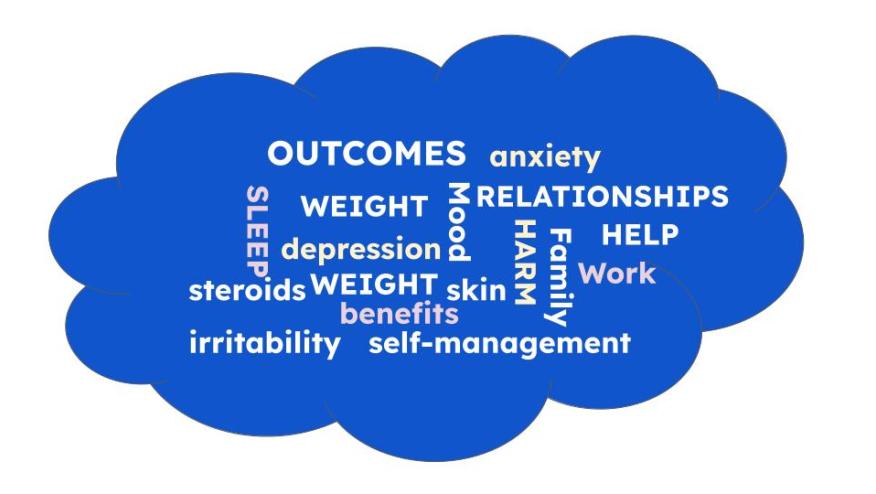
A systematic review and thematic analysis of qualitative and quantitative studies has demonstrated that the impact of glucocorticoid treatment involves physical symptoms, psychological symptoms, effect on participation and contextual factors2. While physical symptoms including weight gain, sleep disturbance and skin changes as well as psychological symptoms such as irritability, depression and anxiety are generally well-appreciated by clinicians, the effects of participation, including impact on work, family, friends, and sexual relationships may be factors we are more likely to overlook. Similarly, in the busy clinic setting, contextual factors such as the often-negative opinions held about glucocorticoids by family, friends, doctors, and the wider community may not be front of mind. On the flip side, is the sense of self-management and mastery patients can experience from being able to manage their disease.
The OMERACT GC Impact group has since published a core outcome set for inclusion in all clinical trials where the effects of GCs are measured3. These include infections, bone fragility, mood disorders, hypertension, diabetes, weight, fatigue, and mortality. The group has recently completed the precise definitions of these core outcomes (keep an eye out for the poster at ACR 2023) in preparation for the next phase of work which will involve the selection of instruments to measure these domains.
Concurrently, an international research team has developed a glucocorticoid treatment-specific patient-reported outcome measure (PRO)4, which will soon be available for licensing and use. The patient-perspective is well recognised as an important quality indicator in both clinical practice and research, and a glucocorticoid PRO will be invaluable for monitoring outcomes in PMR, a condition for which steroid- sparing agents have only recently been shown to be effective.
Patients and clinicians alike, will no doubt benefit from better defined GC outcomes as well as a means of measuring the impact of GC use from the patient-perspective.
References:
1. Black RJ, Robson JC, Goodman SM, et al. A Patient-reported Outcome Measure for Effect of Glucocorticoid Therapy in Adults with Inflammatory Diseases Is Needed: Report from the OMERACT 2016 Special Interest Group. The Journal of rheumatology 2017.
2. Cheah JTL, Robson JC, Black RJ, et al. The patient's perspective of the adverse effects of glucocorticoid use: a systematic review of quantitative and qualitative studies. From an OMERACT working group. Seminars in arthritis and rheumatism 2020; 50(5): 996-1005.
3. Tieu J, Cheah JT, Black RJ, et al. Improving benefit-harm assessment of glucocorticoid therapy incorporating the patient perspective: The OMERACT glucocorticoid core domain set. Seminars in arthritis and rheumatism 2021.
4. Bridgewater S, Shepherd MA, Dawson J, et al. Measuring the impact of steroid therapy on health-related quality of life in patients with rheumatic diseases: international development of a glucocorticoid treatment-specific patient-reported outcome measure. Rheumatology 2023.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.