EMA Final Recommendations on VTE Risk with Tofacitinib Save
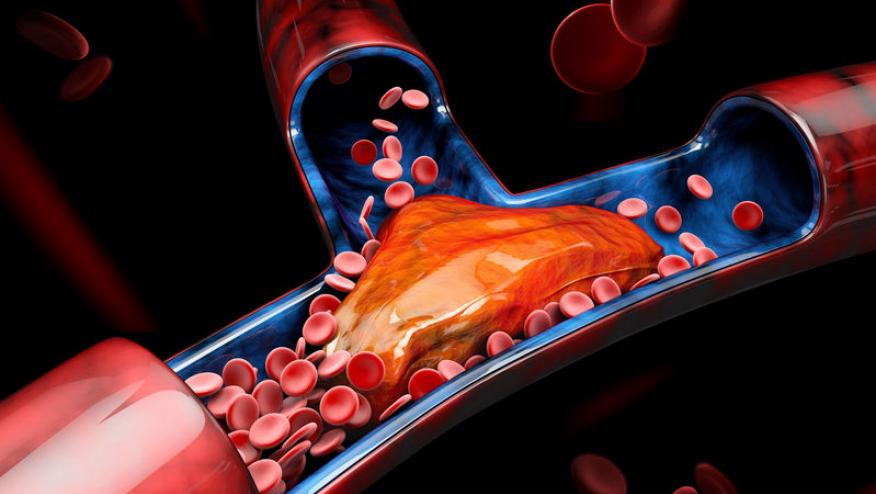
On 14 November 2019 the European Medicines Agency (EMA) concluded that Xeljanz (tofacitinib) could increase the risk of blood clots in the lungs and in deep veins in patients who are already at high risk. These recommendations have been formally published and are intended for EU nations utilizing tofacitinib.
These recommendations are NOT part of the US label, nor are they included in the current prescribing information for tofacitinib.
The EMA recommended that Xeljanz should be used with caution in all patients at high risk of blood clots. In addition, the maintenance doses of 10 mg twice daily should not be used in patients with ulcerative colitis who are at high risk of blood clots unless there is no suitable alternative treatment. Further, EMA recommended that, due to an increased risk of infections, patients older than 65 years of age should be treated with Xeljanz only when there is no alternative treatment.
The Pfizer sponsored study (A3921133) is ongoing and involves patients with rheumatoid arthritis at an increased risk of cardiovascular disease. All data combined showed that the risk of blood clots in deep veins and lungs was higher in patients taking Xeljanz, especially the 10 mg twice daily dose, and in those being treated for an extended period. Results also showed a further increased risk of serious and fatal infections in patients older than 65 years of age.
The recommendations issued by the EMA’s safety committee (PRAC) were endorsed by the Agency’s human medicines committee (CHMP). They replace the temporary measures put in place at the start of the review in May 2019. The European Commission issued its decision approving these changes on 31 January 2020.
The Main Conclusion of Study A3921133
An EMA review has found a dose-dependent increased risk of serious venous thromboembolism (VTE), including pulmonary embolism (PE) (some cases of which were fatal) and deep vein thrombosis in patients taking tofacitinib.
The review considered data from study A3921133, an open-label clinical trial, which was ongoing evaluating the safety of tofacitinib 5 mg twice daily and tofacitinib 10 mg twice daily compared with a tumour necrosis factor (TNF) inhibitor in patients with rheumatoid arthritis. Patients in the study were 50 years of age or older with at least one additional cardiovascular risk factor. After the interim results became available, treatment with tofacitinib 10 mg twice daily was stopped and patients were switched to 5 mg twice daily because of a signal of PE and all-cause mortality. The review also considered additional data from earlier studies.
The review of study A3921133 showed that compared to treatment with a TNF inhibitor, tofacitinib 5 mg twice daily increased the risk of PE about 3-fold while tofacitinib 10 mg twice daily increased the risk roughly 6-fold.
In total there were 17 cases of PE out of 3,123 patient-years with the tofacitinib 10 mg twice daily dose and 9 cases of PE out of 3,317 patient-years with the tofacitinib 5 mg twice daily dose compared with 3 cases out of 3,319 patient-years with a TNF inhibitor. Additionally, there were 28 deaths from all causes out of 3140 patient-years in the tofacitinib 10 mg twice daily arm and 19 deaths from all causes out of 3,324 patient-years in the tofacitinib 5 mg twice daily arm compared with 9 cases out of 3323 patient-years in the TNF inhibitor arm.
As a result, tofacitinib should be used with caution in patients with known risk factors for VTE, regardless of indication and dosage. This includes patients who have:
- heart attack or have heart failure
- cancer
- inherited blood clotting disorders or a history of blood clots
- patients taking combined hormonal contraceptives or hormone replacement therapy
- undergoing major surgery or are immobile
Other risk factors to be considered when prescribing tofacitinib include age, diabetes, obesity (BMI>30), smoking status and hypertension.
The use of tofacitinib 10 mg twice daily for maintenance treatment in patients with ulcerative colitis who have known VTE risk factors is not recommended, unless there is no suitable alternative treatment available.
For treatment of rheumatoid arthritis and psoriatic arthritis, the recommended dose of 5 mg twice daily should not be exceeded.
Patients should be informed about the signs and symptoms of VTE before receiving tofacitinib and be advised to seek prompt medical help if they develop these symptoms during treatment.
Available data also showed that the risk of serious infections and fatal infections was further increased in elderly patients above 65 years of age, as compared to younger patients. Therefore, tofacitinib should only be considered in these patients if no suitable alternative treatment is available.
A letter has been sent to all healthcare professionals expected to prescribe the medicine to inform them of the updated treatment recommendations. The physician’s guide and the patient alert card will be updated with advice to minimise the risk of blood clots.
Select Language for Patients (from EMA)
- Xeljanz could increase the risk of blood clots in patients who are already at high risk.
- If you are being treated with Xeljanz your doctor will review your risk of blood clots and modify your treatment if necessary.
- You may be at high risk of blood clots in the lungs and in deep veins if you have had a heart attack or have heart failure, cancer, inherited blood clotting disorder or a history of blood clots.
- You may also be at risk if you are taking combined hormonal contraceptives or hormone replacement therapy, will have or have recently had major surgery or are immobilised.
- To evaluate the risk your doctor will also consider your age, whether you are obese (your body mass index is above 30), have diabetes, have elevated blood pressure, or smoke.
- If you are at high risk or older than 65 years of age, your doctor may switch your treatment if there is an alternative treatment for you.
- If you are being treated with Xeljanz, you should not change the dose or stop taking the medicine without discussing it with your doctor.
- Ask for medical attention immediately if you develop sudden shortness of breath or difficulty in breathing, chest pain or pain in your upper back, swelling of the leg or arm, leg pain or tenderness, or redness or discoloration in the leg or arm. These may be symptoms of a blood clot in your lungs or veins.
- If you have any concerns about your medicine, you should discuss them with a healthcare professional.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.