Cannabis Arteritis Save
Following the November elections, there are now 29 states and the District of Columbia that have legalized marijuana (aka cannabis) for medical use. Of these, eight states and the District of Columbia have also approved laws legalizing marijuana for recreational use. Regardless of the stated benefits associated with marijuana use, there are potential health risks. One of these which rheumatologists may see more of in the future is cannabis arteritis. The following is a recent case we saw at the University of Colorado.
Case: A 32-year-old man presented with a 5-year history of Raynaud’s phenomenon and a one-year history of increasing digital ulcerations affecting his fingers and toes. He did not smoke or chew tobacco. An evaluation by an outside rheumatologist included an aortic arch and upper extremity angiogram which was interpreted as showing vasculitis of the small and medium-sized vessels of the hand and wrist.
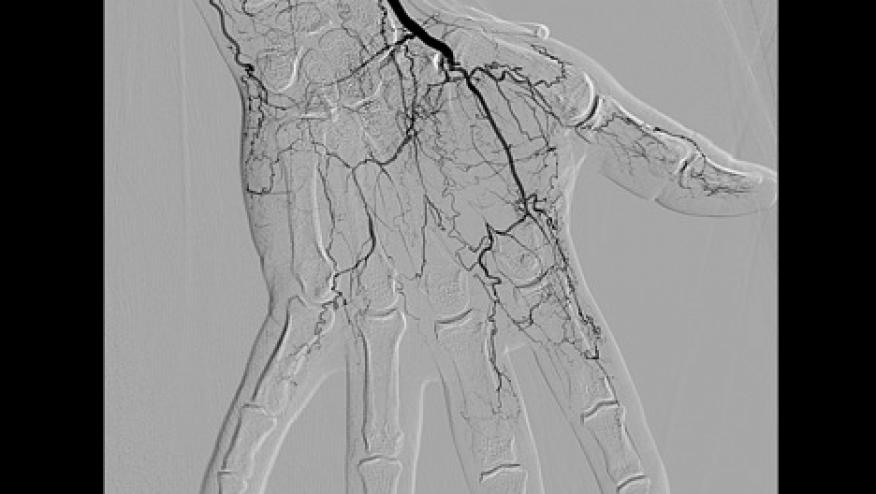
Laboratory evaluation showed normal CBC, chemistries, liver-associated enzymes, urinalysis, sedimentation rate, C-reactive protein, complement levels, ANA, rheumatoid factor, ANCA, cryoglobulins, antiphospholipid antibodies, hepatitis B and C serologies, and SPEP. Urine drug screen was negative except for cannabinoids. He was treated with low dose aspirin, amlodipine, high dose prednisone, and monthly intravenous cyclophosphamide for 4 months. On this therapy, three fingers progressed to gangrene requiring distal phalanx amputation (Figure 1). He was referred and admitted to the University of Colorado hospital. A repeat angiogram of his upper and lower extremities showed multiple distal segmental occlusions and corkscrew collaterals compatible with thromboangiitis obliterans (Figure 2). Further evaluation showed normal lipids, homocysteine, anti-thrombin III activity, and nicotine levels. Anti-prothrombin antibodies and prothrombin gene G20210A mutations were negative.
Questioning about marijuana use revealed he smoked 8-10 “bowls of marijuana” a day (equivalent to a total of 3.5 grams/d = “an eighth of marijuana”). He had smoked marijuana for years and had increased his consumption over the past year to try to help control the pain in his fingers. He consistently denied tobacco use. He was taken off immunosuppressives while continuing antiplatelet agents (aspirin, clopidogrel) and vasodilators. Importantly, after prolonged discussion and counselling he stopped smoking marijuana. His arteriopathy slowly stabilized but he is left with significantly impaired hand function and cold sensitivity of his digits.
Figure 1: Right hand digital infarctions and gangrene.

Figure 2: Right hand angiogram with absent ulnar artery, poor blood flow to digits, and cork-screw collaterals.

Marijuana is the most commonly used illicit drug in the United States as well as worldwide. In the U.S., approximately 20 million individuals (7.5% of population aged 12 or older) are current users with 6-7 million (2.5% of population) being chronic daily users (Azofeifa A, et al. MMWR 65 (11): 1-25, 2016). Chronic use of marijuana has been associated with a number of health concerns. Cardiovascular complications including acute myocardial infarction, transient ischemic attacks, and a peripheral arteriopathy have been reported (Jouanjus E, et al. J Am Heart Assoc 2014; 3:e000638 doi:10.1161/ JAHA.113. 000638). The peripheral arteriopathy has been called cannabis arteritis (Cottencin O, et al. J Addict Med 4: 191, 2010).
Cannabis arteritis (CA) resembles thromboangiitis obliterans (TAO) (aka Buerger’s disease) and both should be considered in young adults less than age 50 presenting with peripheral vascular disease. Over 20% of lower extremity arteriopathy in young adults is due to TAO and/or CA. The clinical and arteriographic presentations of TAO and CA are nearly identical. Both cause a nonatheromatous peripheral arteriopathy with segmental and multifocal involvement of the small and medium-sized arteries distal to the elbow and knee. Superficial vein thrombosis has also been reported. Both diseases predominantly affect young males and can cause gangrene of the digits. Laboratory evaluation is frequently unremarkable including normal acute phase reactants.
Histopathologic examination of amputated digits shows thrombosis with a secondary inflammatory response (Disdier P, Constans J. Presse Med 29: 2226, 2000). This explains why immunosuppressive medications are ineffective and smoking cessation of both tobacco and marijuana coupled with antiplatelet therapy and vasodilators (oral and IV) is the recommended treatment regimen. Despite treatment, up to 30% of patients require amputation of one or more digits.
Distinguishing CA from TAO can be difficult since they have similar presentations and 97% of cannabis users also smoke tobacco. However, as demonstrated in our case, at least 3% of patients with CA do not smoke tobacco suggesting cannabis can cause an arteriopathy in someone who does not smoke tobacco. The average intake of those who develop CA is 3-4 “joints” a day for at least a year. Alternatively, a prior study reported that over 20% of patients with TAO due to tobacco smoking also were chronic cannabis users (Sauvanier M, et al. J Mal Vasc 27: 69, 2002). Consequently, there may be a synergistic interaction between tobacco smoke and cannabis which contributes to some patients developing a peripheral non-atheromatous arteriopathy.
The etiology of CA is poorly understood. The main active ingredient in cannabis is Δ9-transtetra- hydrocannabinol (THC). A typical “joint” contains between 0.5 and 1.0 gram of cannabis plant matter, which varies in THC content between 5 and 150 milligrams. One “bowl” of marijuana contains about 0.35 grams of cannabis with a variable THC content typically less than 50 milligrams. During combustion 15-60% of THC is absorbed. Notably cannabis/marijuana smoke contains 421 other chemical components, many of which are the same toxic substances present in tobacco smoke.
THC and some of these other substances may have direct toxic effects on blood vessels. In addition, activation of cannabinoid (CB1) and non-cannabinoid receptors on endothelial cells can cause increased production of reactive oxygen species and decreased nitric oxide production. This could potentially lead to endothelial cell injury, vasoconstriction, and thrombosis. Since cannabis users may also abuse other illicit drugs with vascular effects (methamphetamines, cocaine, etc.), this possibility must also be considered.
A legitimate but unanswerable question is - given the high frequency of marijuana and tobacco use, why are there so few cases of CA or TAO? Clearly more research needs to be done. In the meantime, it is important for rheumatologists to consider cannabis use in all patients presenting with a distal peripheral arteriopathy resembling TAO whether or not the patient smokes or chews tobacco.
This can only be uncovered if you specifically ask the patient: “Do you smoke marijuana (or weed, pot, grass, Mary Jane, ganja, herb, hash, skunk, chronic, reefer, 420, etc.)”?











If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.