EULAR Recommendations on Sjögren’s Syndrome Save
The European League Against Rheumatism (EULAR) has established an international collaborative group (EULAR SS Task Force) to develop the first EULAR evidence and consensus-based recommendations for the management of patients with Sjogens syndrome (SjS).
The Task Force included specialists in rheumatology, internal medicine, oral health, ophthalmology, gynaecology, dermatology and epidemiology, statisticians, general practitioners, nurses and patient representatives from 30 countries of the 5 continents.
A literature review, grading process and consensus was reached regarding treatment. The results included 3 overarching, general consensus-based recommendations and 12 specific recommendations. These guidelines address Sicca symptoms and the management of systemic disease. Specifically addressing the use of topical oral (saliva substitutes) and ocular (artificial tear drops, topical non-steroidal anti-inflammatory drugs, topical corticosteroids, topical CyA, serum tear drops) therapies, oral muscarinic agonists (pilocarpine, cevimeline), hydroxychloroquine, oral glucocorticoids, synthetic immunosuppressive agents (cyclophosphamide, azathioprine, methotrexate, leflunomide and mycophenolate), and biological therapies (rituximab, abatacept and belimumab).
Overarching Recommendations
- Patients with SjS should be managed at, or in close collaboration with, centres of expertise following a multidisciplinary approach
- The first therapeutic approach for dryness should be symptomatic relief using topical therapies
- Systemic therapies may be considered for the treatment of active systemic disease
Specific Recommendations
- Baseline evaluation of salivary gland function is recommended before starting treatment for oral dryness
- The preferred first therapeutic approach for oral dryness according to salivary gland function may be: a) Non-pharmacological stimulation for mild dysfunction; b) Pharmacological stimulation for moderate dysfunction; and c) Saliva substitution for severe dysfunction
- The first-line therapeutic approach to ocular dryness includes the use of artificial tears and ocular gels/ointments
- Refractory/severe ocular dryness may be managed using topical immunosuppressive-containing drops* and autologous serum eye drops
- Concomitant diseases should be evaluated in patients presenting with fatigue/pain, whose severity should be scored using specific tools
- Consider analgesics or other pain-modifying agents for musculoskeletal pain, considering the balance between potential benefits and side-effects
- Treatment of systemic disease should be tailored to organ-specific severity using the ESSDAI definitions
- Glucocorticoids should be used at the minimum dose and length of time necessary to control active systemic disease
- Immunosuppressive agents should be mainly used as GC-sparing agents, with no evidence supporting the choice of one agent over another
- B-cell targeted therapies may be considered in patients with severe, refractory systemic disease
- The systemic organ-specific therapeutic approach may follow, as a general rule, the sequential (or combined) use of GCs, immunosuppressive agents and biologics
- Treatment of B-cell lymphoma should be individualised according to the specific histological subtype and disease stage
The Research Agenda (as yet unmet needs)
- Is there a specific, differentiated treatment of lymphomas related to SjS?
- Is combination therapy a potential intervention to explore in SjS?
- Exploring targeted therapies against Th17 cytokines, IFNα, RORɣt expression, Janus kinases (JAKS), STATs and mTOR intracellular pathways or interleukin-1.
- Searching for predictive factors of biological response.
- Potential use of sequential or intralesional use of biological therapies.
- Encouraging the development of new and innovative therapies.
- In what proportion of systemic patients is induction therapy with current therapeutic options effective in inducing sustained remission?
- Is the use of immunosuppressive and biologic agents safe and efficacious in the absence of concomitant glucocorticoid treatment?
- How safe and efficacious is the off-label use of other biologics after rituximab has failed?
- Can we find predictors of differential response to the synthetic and biological drugs used in SjS?
- Can we predict who will maintain remission after withdrawal of glucocorticoids?
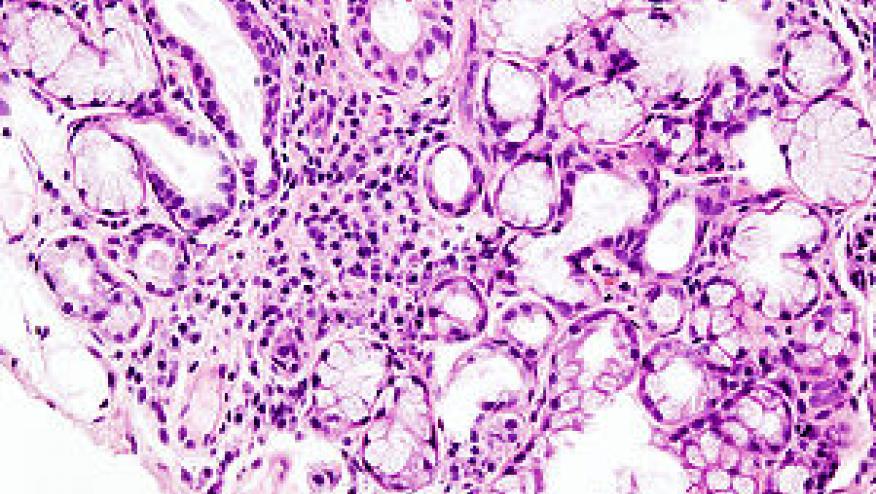
- Will we be able to develop precision (personalised, stratified) medicine approaches in SjS? (IFN signature +/-; immunological or histopathological markers +/-)?
- Which biomarkers will help identify better predictors of poor outcomes?










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.