ACR Newly Revised COVID-19 Vaccine Clinical Guidance for RMD Patients Save
The ACR has updated its clinical guidance for the use of COVID-19 vaccination in patients with musculoskeletal disorders (MSK).
Summary of Guidance documents and versions
This summary was initially approved by the ACR Board of Directors on February 8, 2021 and updated on March 4, 2021. A full paper (Version 1), was published in Arthritis & Rheumatology on May 24, 2021.*
New recommendations regarding mycophenolate, methotrexate, acetaminophen, and NSAID timing considerations+ were added to this summary on April 28, 2021 and were added to the full paper (Version 2), which was published in Arthritis & Rheumatology on June 15, 2021.**
Updated recommendations regarding age restrictions, preferences between specific vaccines, and need for continued preventive measures were added to this summary on June 19, 2021 and were added to the full paper (Version 3), which was published in Arthritis & Rheumatology on August 4, 2021.***
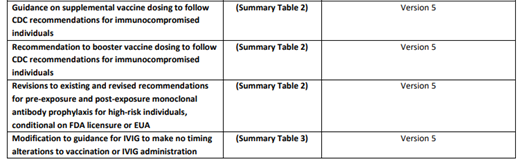
Updated recommendations regarding preference for use of mRNA vaccines, use of a supplemental vaccine dose (i.e., ‘booster’) and associated temporary interruption of immunomodulatory medications, and the FDA EUA for postexposure prophylaxis with monoclonal antibody treatment for vaccinated AIIRD patients were added to this summary on August 19, 2021. These recommendations were added to the full paper (Version 4), which will be submitted to Arthritis & Rheumatology for publication.
Updated recommendations for supplemental (booster) dosing and revised information for holding immunomodulatory medications were added to the version 4 summary on October 27, 2021 and December 15, 2021. These recommendations were added to the full paper (Version 4), which will be submitted to Arthritis & Rheumatology for publication.
Updated recommendations differentiating supplemental and booster doses, including timing considerations, were added to the version 5 summary on January 28, 2022. Revised guidance is also provided related to pre- and post-exposure prophylaxis with monoclonal antibody treatment, considering updated EUAs. These recommendations were added to the full paper (Version 5), which will be submitted to Arthritis & Rheumatology for publication.
Purpose
The purpose of this document is to provide guidance to rheumatology providers on the use of the COVID-19 vaccine and the associated management of rheumatic and musculoskeletal disease patients around the time of vaccination against SARS-CoV-2. These statements were based upon a dearth of high-quality data and are not intended to replace clinical judgment. Modifications made to treatment plans, particularly in complex rheumatic disease patients, are highly disease-, patient-, geography-, and time-specific and, therefore, must be individualized as part of a shared decision-making process. This guidance is provided as part of a ‘living document,’ recognizing rapidly evolving evidence and the anticipated need for frequent updates as such evidence becomes available.
Methods
The North American Task Force panel, consisting of 9 rheumatologists, 2 infectious disease specialists, and 2 public health experts with current or past employment at the Centers for Disease Control (CDC), convened multiple times in December 2020 and January 2021. The Task Force proposed a variety of clinical questions related to COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases (RMD), divided itself into subgroups (i.e., teams), and assigned the clinical questions to the various teams by topic (e.g., vaccine effectiveness, safety). Each team was charged to generate an evidence review covering that topic; the evidence reviews were combined into an evidence summary document that was collated and disseminated to the entire Task Force. The Task Force reviewed the clinical questions and associated proposed vaccine guidance statements that were evaluated using a well-established method of consensus building (modified Delphi process). This process included two rounds of asynchronous anonymous rating by email and two live Version 5 Revised January 28, 2022 2 webinars including the entire Task Force. Panel members rated their agreement with draft statements using a numeric scoring system, and consensus was determined to be either “moderate” (M) or “high” (H), based on the dispersion in the rating results. To be approved as guidance, median ratings were required to correlate to pre-defined levels of agreement (with median values interpreted as “agreement,” “uncertainty” or “disagreement”) with either moderate or high levels of consensus based on the statements as they were originally voted upon, unless they were subsequently reconsidered. For this summary document, several rating statements that wer
Results and Conclusion
General considerations related to COVID-19 vaccination in rheumatic and musculoskeletal disease patients are shown in Table 1. Statements more specific to patient groups, as well as general disease- and timing-related considerations, are presented in Table 2. No evidence was found to support a concern regarding the use or timing of immunomodulatory therapies in relation to vaccine safety. Therefore, guidance regarding immunomodulatory medication and vaccination timing (Table 3) was given considering the intent to optimize vaccine response. An important set of guiding principles, foundational assumptions and limitations are mentioned in the Supplemental Table. The ACR is committed to updating this guidance as a ‘living document’ as new evidence emerges. Statements in bold are those that have been revised or added in the most current version of the document. These changes are also summarized in the Appendix Table. (see the ACR link for the Appendix Tables)
What has been added to prior guidance?









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.