Anti-TNF and CNS Events: The Link Strengthens Save
Patients with autoimmune diseases who were treated with tumor necrosis factor (TNF) inhibitors had an increased risk of developing inflammatory central nervous system (CNS) adverse events, a nested case-control study found.
Among patients with diseases such as rheumatoid arthritis (RA), psoriasis, and ulcerative colitis who were exposed to TNF inhibitors, there was a three-fold increased risk of any inflammatory CNS event in the study's primary analysis, with an adjusted odds ratio of 3.01 (95% CI 1.55-5.82, P=0.001), according to Andrew McKeon, MD, of the Mayo Clinic in Rochester, Minnesota, and colleagues.
And the risk was almost five-fold higher among the subgroup of patients with RA specifically, with an adjusted OR of 4.82 (95% CI 1.62-14.36, P=0.005), the researchers reported in JAMA Neurology.
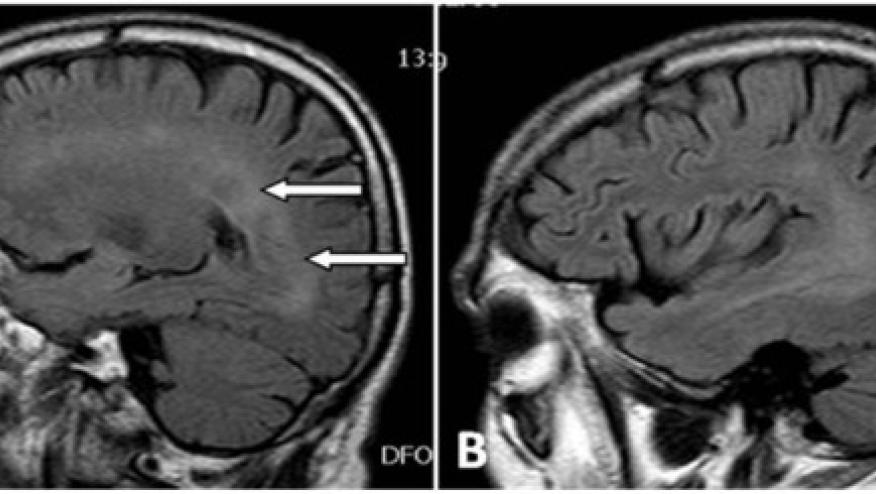
A link between TNF inhibitors and demyelinating CNS events has been suspected since shortly after those agents became available more than 20 years ago. These events included multiple sclerosis (MS), optic neuritis, transverse myelitis, and neuromyelitis optica spectrum disorder. In a Spanish registry, there have been 740 reports of demyelinating events, 254 of which were MS, and 358 cases of optic neuritis.
There also have been reports of inflammatory nondemyelinating CNS events such as neurosarcoidosis and CNS vasculitis, although less is known about these events.
To explore these potential associations in a large population, McKeon and colleagues examined the electronic health record system of the Mayo Clinic's three locations (Rochester; Scottsdale, Arizona; and Jacksonville, Florida) for the years 2003 to 2019.
The study population included more than 32,000 patients who had been diagnosed with RA, psoriasis, psoriatic arthritis, ankylosing spondylitis, Crohn's disease, or ulcerative colitis, and who had been treated with any disease-modifying therapy. They identified 106 patients who developed CNS events, matching them with 106 controls who had the same autoimmune diseases but without CNS events.
Two-thirds of the patients were women. Median age was 36 at the onset of the autoimmune disease for patients and 35 for controls, and median disease duration was 12 years for patients and 13 years for controls. The most common diagnosis was RA in 45%.
Inflammatory demyelinating events developed in 56 patients, with most being MS, and inflammatory nondemyelinating events such as aseptic meningitis, CNS vasculitis, and idiopathic leptomeningitis were reported in 50.
Among the 106 patients who developed CNS events, 60% had been exposed to any of the available TNF inhibitors, which were etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), golimumab (Simponi), and certolizumab pegol (Cimzia). Among the control group, 40% had received anti-TNF treatment.
Among the patients who had demyelinating events, 70% had anti-TNF exposure compared with 50% of controls, while of those who had nondemyelinating events, 50% of patients were exposed compared with 28% of controls.
When the analysis was stratified according to the type of CNS event, similar results were seen as in the primary analysis:
- Inflammatory demyelinating CNS events: adjusted OR 3.09 (95% CI 1.19-8.04, P=0.02)
- Inflammatory nondemyelinating CNS events: adjusted OR 2.97 (95% CI 1.15-7.65, P=0.02)
Unlike the RA subgroup, a pooled analysis of patients with ankylosing spondylitis, psoriasis, psoriatic arthritis, Crohn's disease, and ulcerative colitis found no significant risk of inflammatory CNS events (OR 2.13, 95% CI 0.90-5.05, P=0.09).
In 90% of patients who developed the neurologic symptoms, anti-TNF exposure took place within 1 year of the symptom onset, suggesting a temporal association, the researchers noted.
"We hypothesized that TNF inhibitors may further dysregulate already aberrant immune responses, triggering inflammatory CNS events in patients with certain autoimmune diseases," they wrote.
The TNF cytokine has multiple functions ranging from immune regulation to inhibition of tumor cells and defense against pathogens. "Proposed mechanisms for the paradoxical development of inflammatory CNS events in association with TNF inhibitor exposure include immune dysregulation from the inhibition of apoptosis of autoreactive T cells, which may then enter the CNS and cause demyelination," they explained.
They also emphasized that the TNF inhibitors are highly effective therapies for these diseases, and the CNS events are uncommon, and also acknowledged that their study does not imply causality.
"Further research is needed to explore whether this association indicates de novo inflammation or exacerbation of already aberrant inflammatory pathways," they concluded.
In an accompanying editorial, Jeffrey M. Gelfand, MD, and Jinoos Yazdany, MD, of the University of California San Francisco cautioned that "the effect size reported in the study should be interpreted with some caution," because the analysis did not adjust for severity of underlying disease. "It is plausible that individuals with more severe autoimmune diseases were both more likely to receive biological agents such as TNF inhibitors and more prone to develop neuroinflammatory events," the editorialists wrote.
"The next steps should include population-based observational studies that control for disease severity," they wrote.
Disclosures
The study was funded by the National Center for Advancing Translational Sciences.
The authors disclosed relevant relationships with Biogen, Pfizer, Genentech, AbbVie, Sanofi-Genzyme, Alexion, Viela Bio, Union Chimique Belge, Astellas, Griffols, Autoimmune Encephalitis Alliance, Chugai/Roche, Mitsubishi Tanabe, Novartis, Caladrius, Brainstorm Therapeutics, Roivant, Euroimmun, and Medimmune.
Primary Source
JAMA Neurology
Secondary Source
JAMA Neurology










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.