Diagnosis and Management of Kawasaki Disease Save
The journal Circulation has published a comprehensive overview called “Update on Diagnosis and Management of Kawasaki Disease,” summarizing data published since the 2017 American Heart Association Scientific Statement on Kawasaki Disease related to diagnostic criteria, risk scores and treatment options for children and adults with this condition.
Advances in cardiac imaging techniques and risk categorization have led to improvements in diagnosis, initial treatment and long-term management of patients with Kawasaki Disease.
Statement highlights include:
- Kawasaki Disease is a rare but serious illness primarily affecting children younger than five years old. The disease can cause inflamed blood vessels throughout the body, and it is the leading cause of acquired (not congenital) heart disease in children throughout the developed world.
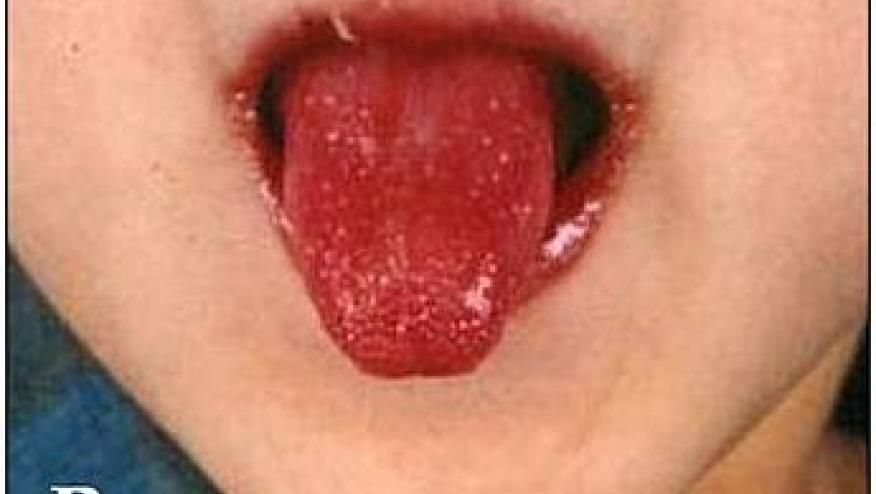
- Although the cause of Kawasaki Disease is still unknown, however, there is a strong suspicion that the cause is infectious but no single infectious agent has been implicated. Health care professionals diagnose Kawasaki Disease based on a set of well-established symptoms, including prolonged fever, rash, reddened eyes and swelling of the hands and feet. Without timely treatment, one in four children can develop coronary artery dilation and/or coronary artery aneurysms.
- Health care professionals use coronary artery Z-scores, a measurement that compares the coronary artery diameter of a child with Kawasaki Disease to the expected diameter of coronary arteries in healthy children of similar age, sex and body size to evaluate coronary abnormalities and classify risk. Children with Z-scores greater than 2.5 are at increased risk for developing coronary artery aneurysms. Although a Z-score alone should not determine the damage to coronary arteries, the statement highlights the need for consistent Z-score equation over time to ensure a patient’s risk classification does not change.
- Early identification of children with Kawasaki Disease at risk of developing coronary artery aneurysms remains a challenge in a multiethnic population and it is critical to diagnose Kawasaki Disease early for optimal management. A new risk scoring system specific to children in North America combines factors like age younger than six months, Asian race, elevated coronary artery Z-scores of at least 2 and higher C-reactive protein levels (a substance in the blood that is elevated when there’s inflammation in the body). These advancements help clinicians identify high-risk patients who might require more intensive initial treatment to potentially reduce coronary artery complications.
- The statement suggests echocardiograms at regular time intervals, with a higher frequency in patients with coronary artery Z-scores greater than 2.5, to track the progression of any coronary artery abnormalities during hospitalization or after discharge. Echocardiographic, or heart ultrasound, techniques have improved since 2017 to better detect coronary artery dilation or aneurysms, which can help patients avoid more serious and/or long-term heart problems.
- Intravenous immunoglobulin (IVIG), a mixture of antibodies and proteins to help fight infections, remains the standard of care for patients with Kawasaki Disease. Studies have shown, however, that dosing adjustments based on lean body mass in patients with obesity can help reduce the risks of complications.
- The statement reevaluates the use of aspirin during the acute phase of Kawasaki Disease. Recent studies have shown using low- or medium-dose aspirin may be just as effective as high-dose aspirin. Ongoing trials are comparing different doses to confirm these results.
- Recent studies have found adding other therapies, such as corticosteroids or infliximab, can help children with Kawasaki Disease who are at high risk for IVIG resistance. These new options may be effective in preventing coronary artery complications and offer health care professionals more options in managing treatment-resistant cases.
- For children with Kawasaki Disease who have larger coronary aneurysms, blood-thinning medications like aspirin (typically 81 mg daily) combined with anticoagulants, such as warfarin or low molecular weight heparin, may help prevent dangerous blood clots. Recent evidence indicates that using direct oral anticoagulants in the treatment of patients with large coronary artery aneurysms may be more effective and safer, require less monitoring and have fewer side effects, however, further research is needed to confirm these findings.
- The outbreak of COVID-19 saw an increase in a related condition called Multisystem Inflammatory Syndrome in Children (MIS-C). MIS-C became a diagnostic challenge since many symptoms including fever, rash and heart-related issues, overlap with symptoms of Kawasaki Disease. New data have helped differentiate the two conditions by identifying additional symptoms of MIS-C that include gastrointestinal issues, a low number of platelets that could cause bruising or bleeding, and a lower than normal number of white blood cells. In contrast, coronary artery involvement remains a hallmark of Kawasaki Disease, helping health care professionals make more accurate diagnoses. Machine learning algorithms have also been developed that may help clinicians distinguish between Kawasaki Disease and MIS-C.
- All medical centers with patients with Kawasaki Disease and giant coronary artery aneurysms need to have a multidisciplinary heart team and a protocol in place to address major adverse cardiac events.
- This updated scientific statement highlights the need for a formal transition program to ensure continuity of care for adolescents and adults with a history of Kawasaki Disease. Patients with giant aneurysms remain at high risk for heart attack and require lifelong monitoring and care. Further research is needed to optimize the timing and methods used to monitor long-term heart health in patients with the disease.
- Individuals with Kawasaki Disease who plan on becoming pregnant are at high risk for adverse cardiac events and require care from obstetricians who have knowledge of Kawasaki Disease in tandem with consultations with a cardiologist.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Rheumatic Feber, Endocarditis, and Kawasaki Disease Committee of the Council on Lifelong Congenital Heart Disease and Heart Health in the Youn; the Council on Cardiovascular and Stroke Nursing; the Council on Cardiovascular Radiology and Intervention; and the Council on Clinical Cardiology. American Heart Association scientific statements promote greater awareness about cardiovascular diseases and stroke issues and help facilitate informed health care decisions. Scientific statements outline what is currently known about a topic and what areas need additional research. While scientific statements inform the development of guidelines, they do not make treatment recommendations. American Heart Association guidelines provide the Association’s official clinical practice recommendations.
Statement writing group authors and their disclosures are listed in the manuscript.
The Association receives funding primarily from individuals. Foundations and corporations (including pharmaceutical, device manufacturers and other companies) also make donations and fund specific Association programs and events. The Association has strict policies to prevent these relationships from influencing the science content. Revenues from pharmaceutical and biotech companies, device manufacturers and health insurance providers, and the Association’s overall financial information are available here.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.