Disease Modification, Disparities and the Next Therapeutic Frontier in Gout Save
Gout management has entered what Dr. Robert Terkeltaub MD from UC San Diego described as its “disease-modifying era,” during his talk at RheumNow Live 2026 In a recent comprehensive review of the past, present, and future of gout therapy, the central message was clear: “We can really apply disease modification to gout based on prospective, randomized controlled trials.”
In controlled settings, treat-to-target urate lowering works. When allopurinol or febuxostat is titrated appropriately, 80–90% of patients can achieve a serum urate <6 mg/dL. Imaging confirms that sustained urate control reduces crystal burden, shrinks tophi, and improves structural outcomes. Dual-energy CT demonstrates that “when you see melting of tophi, you get pretty impressed that you’re modifying disease.”
Yet the real-world picture diverges sharply. “Oral treat-to-target urate lowering therapy is an absolute bust in the real world,” the speaker emphasized. In primary care—where most gout is managed—only 20–30% of patients reach target urate. Dose inertia remains common; 300 mg/day of allopurinol is often treated as a ceiling, despite evidence that mean effective doses are closer to 400–500 mg/day.
Healthcare disparities compound the challenge. Minority populations experience inferior gout outcomes, and pharmacogenomic variability—including ABCG2 transporter polymorphisms—contributes to allopurinol resistance. Meanwhile, allopurinol hypersensitivity syndrome (AHS) remains a feared complication. Although rare, AHS carries an estimated 25% mortality rate. Emerging data suggest that JAK inhibition may mitigate the type I/II interferon–driven cytokine storm characteristic of severe cutaneous reactions—a potential paradigm shift for a historically devastating condition.
Cardiovascular risk is another underappreciated dimension. “Recent gout flare [is] a doubling of the risk of myocardial infarction or stroke,” with a fivefold increase in fatal events. Colchicine, now FDA-approved for secondary cardiovascular prevention, offers dual benefit. Retrospective data show improved major adverse cardiovascular event outcomes when colchicine is combined with urate-lowering therapy. However, uptake remains limited.
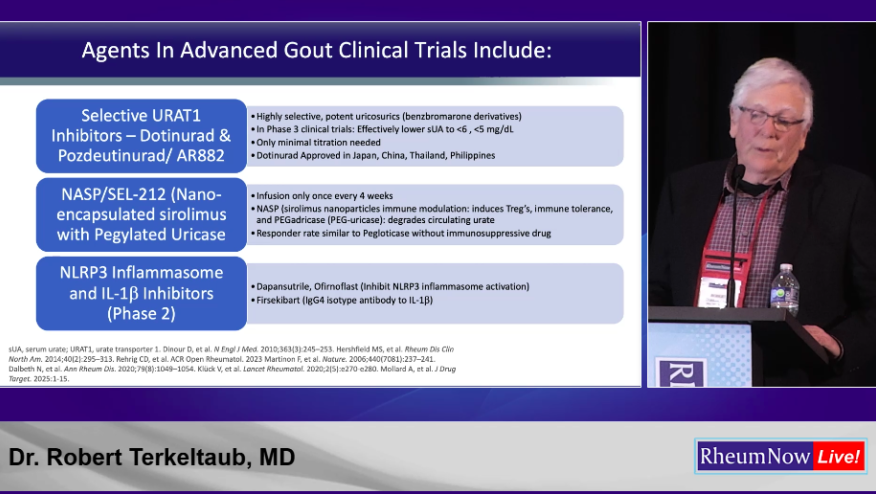
Novel therapeutics are reshaping the landscape. SGLT2 inhibitors lower serum urate by approximately 1 mg/dL and reduce flares and mortality in gout cohorts. Pegloticase durability has improved with concomitant immunosuppression, increasing treatment completion rates to over 70%. Meanwhile, selective URAT1 inhibitors and IL-1β–targeted agents are advancing through late-stage trials, promising more effective flare prophylaxis and urate reduction.
Key Takeaways for Clinical Practice
• Treat-to-target urate lowering is disease-modifying—but underutilized in real-world settings.
• Baseline serum urate >9 mg/dL predicts significantly worse long-term outcomes and hospitalization risk.
• Gout flares are not benign; they are linked to increased cardiovascular events and mortality.
• Colchicine prophylaxis and cardiovascular protection remain underused tools.
• Emerging pharmacogenomics and pipeline therapies offer hope for refractory disease and treatment-resistant patients.
The field has evolved from symptomatic control to disease modification. The challenge now is translating ideal-trial success into equitable, durable real-world outcomes.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.