Do Probiotics Improve Psoriatic Arthritis? Save

The following is a true account of this morning and every other morning I can remember.
The first one to greet me when I wake up is our cat. As a matter of fact, he’s the one who typically wakes me up. For the next hour as I try to gather my senses, he’s chirping at me and following me incessantly. Why? He’s become accustomed to (or maybe he’s trained us?) to feed him his probiotic first thing in the morning. This came at the advice of his veterinarian due to some GI issues he’s had in the past. Finally when that little packet of powdered bacteria is poured into his bowl, there is peace.
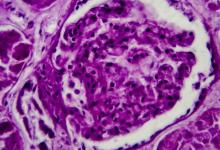
As in the world of felines, psoriatic arthritis and the gut microbiome have become more intertwined, especially in the past few years. It was to my amazement that one of the first abstracts I came across was the effect of probiotic modulation on gut dysbiosis and disease activity in psoriatic arthritis patients.
The topic of probiotics and gut microbiome is not only a hot topic in the research world but also amongst patients. It is not unusual that one of the first questions I receive after relaying the news of the diagnosis of psoriatic arthritis is, “Doc, is there anything I can eat or not eat to make this better.” Probiotics can be seen as a simple solution. First of all, it has “pro” in its name so it must be good, right? I think it also allows the patient to have control, where they can tailor their diet or even approach therapy in a much more “natural” way. Lastly, I think the general public is starting to realize that the foods we’ve been putting in our stomachs for the past few decades may not have been the healthiest, and we are seeing a trend from less of a “fast-food” diet and more organic and gut friendly.
Abstract #0778 was a double-blind randomized controlled trial, which recruited 65 patients with psoriatic arthritis where roughly half received placebo and another half received a probiotic containing bifidobacterium and lactobacillus. After 24 weeks, these patients’ clinical assessment, stool, serum and immune cell composition were collected.
There was no difference in the probiotic group compared to the placebo group in terms of disease activity. In terms of assessing for stool microbiome and dysbiosis, levels of zonulin, calprotectin and anti-trypsin were assayed to measure gut permeability and intestinal inflammation. There was a difference in zonulin levels in the probiotic group but a similar albeit smaller difference was seen in the placebo group. Otherwise, there were limited effects on the dysbiosis of the gut. Lastly, there were minor effects on T cell composition with no differences in Th1, Th17, Treg cells.
Although the results were not as promising as one would have hoped, I do believe studies like this should continue, especially with the availability of gene sequencing lending to more potential targets in the future. Furthermore, this study was hindered by its relatively small sample size and short trial period. My final thought is although I can’t full-heartedly recommend probiotics to aid my psoriatic arthritis patients; should I stop giving probiotics to our cat? Do I dare?









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.