Dress Syndrome – A Diagnostic and Management Nightmare Save
21 yr. old woman presented to the Emergency Department (ED) with chest pain and dyspnea.
She went to her family physician 12 weeks earlier for acne and was prescribed minocycline. Six weeks later, she developed a diffuse pruritic skin rash accompanied by low grade fever and was evaluated in the ED where she was found to have a white blood cell count of 45.1 with 37% eosinophils and 10% atypical lymphocytes. The minocycline was stopped and she was started on prednisone 40 mg per day.
She was evaluated by a dermatologist 3 days later who performed a skin biopsy that confirmed the diagnosis of DRESS (drug rash with eosinophilia and systemic symptoms). The prednisone was increased to 60 mg per day and she was told to decrease the dose by 10 mg every week until off. The skin rash resolved and she felt well until she reached a dose of 30 mg per day. Several days later, developed chest pain and dyspnea. In the ED she went into cardiac arrest and was resuscitated after 20 minutes. An echocardiogram showed hypokinesia of the left ventricle and a CT scan of the chest did not reveal a pulmonary embolus. She was placed on ECMO for 3 weeks and treated with high dose steroids, IVIG and Anti-Thymocyte Globulin (ATG). An endomyocardial biopsy showed diffuse active myocarditis with coagulative myocyte necrosis and a mixed infiltrate including eosinophils - all consistent with DRESS myocarditis. She was maintained on ECMO for 2 weeks and also dialyzed for acute renal failure. Gradually the heart function improved to an EF of 23%, but she remains on dialysis. She is currently on prednisone, cyclosporine and mycophenolate mofetil.
DRESS SYNDROME
DRESS syndrome is but one of a group of disorders falling under the heading of severe cutaneous adverse reactions (SCARs), which includes Stevens-Johnson syndrome, toxic epidermal necrolysis (TENS), DRESS and acute generalized exanthematous pustulosis. Each of these is rapid, progressive and carries significant systemic morbidity and mortality risks. DRESS is rare and thought to have incidence of 1 per 1,000 to 10,000 exposures and its mortality is 10%-20%. The etiology is multifactorial and may involve multiple immune reactions, ethnic predisposition, genetically determined enzyme deficiencies and reactivation of herpes viruses (HHV-6, HHV-7, EBV, CMV).
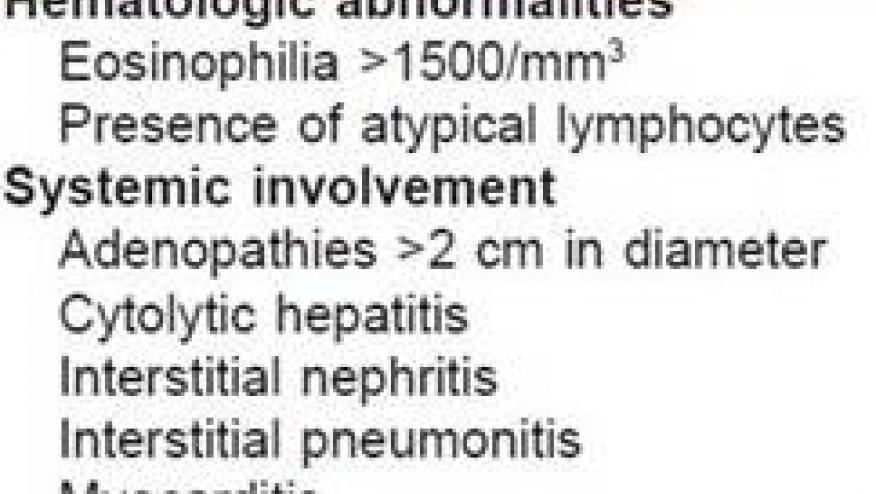
DRESS is an idiosyncratic reaction (type B), characterized by peripheral eosinophilia and systemic symptoms that include fever, rash, lymphadenopathy, hepatitis, atypical lymphocytes and elevation of hepatic enzymes (ALT >100 U/L). Patients may appear septic or rapidly progress to multi-organ failure. Commonly implicated drugs include allopurinol, sulfonamides, anticonvulsants (phenytoin, phenobarbital, carbamazepine), antiretrovirals (abacavir and nevirapine) and minocycline. The diagnosis is difficult or delayed as DRESS often mimics other serious systemic disorders such as lupus, thrombotic thrombocytopenic purpura, EGPA, vasculitis and the hemophagocytic syndrome. The long latency period between start of drug intake and the initial manifestation of DRESS and the successive onset of skin and organ involvement complicates the early diagnosis. The clinical course may be prolonged, often with flares, even after drug discontinuation. Treatment is based on steroids and on the suspension of the suspect drug.
This case underscores the devastating consequences of DRESS Syndrome. An accurate diagnosis was reached rapidly based on clinical features of a morbilliform rash, fever, atypical lymphocytosis and eosinophilia within 6 weeks of starting minocycline; the drug was stopped and steroids initiated. Despite these actions, fulminant myocarditis developed during the steroid taper, a well-recognized but rare complication of DRESS Syndrome. Patients who present with DRESS Syndrome may require hospitalization to fully evaluate the extent of major organ involvement and certainly close follow-up following cessation of the offending drug is critical. Although oral corticosteroids are frequently prescribed, no formal evidence supporting efficacy has been reported.









