Hot Stuff Part IV: Cardiovascular Outcomes and Vasculitis Save
Read Part I: Hot Stuff from the Cleveland Clinic's Biologic Therapies Summit
Read Part II: Current Status and Recommendations on Vaccines and Biologics
Read Part III: Zoster and Biologics: Special Considerations
Dr. Elaine Husni – Reducing Cardiovascular Risks in Practice
Dr. Husni reviewed the growing body of research regarding cardiovascular disease and the high frequency of cardiovascular events (CVE), myocardial infarctions and altered mortality rates (SMR) with inflammation or drug therapy. The CV risk appears to be driven by the chronic inflammatory burden seen with diseases like RA, PsA, IBD, etc.
-
There are more than 20 studies showing an increased mortality in RA (largely due to CVD). This results in a 3-18 yr. reduced life expectancy.
-
Elevated ESR, CRP and the shared epitope are associated with CV risk.
-
CCP antibodies are associated with increased risk of ischemic heart disease.
-
This same risk has been seen in patients with PsA and psoriasis.
-
There is controversy about the protective effects of low dose ASA use. Clearly ASA indicated in those with history of CV events or at risk. Primary prevention in low/no risk populations, including RA patients, is unclear.
-
Unclear whether selective COX-2 inhibitors are equivalent or safer than nonselective NSAIDs.
-
PRECISION trial is underway will examine if there is a difference in CV outcomes when RA (or OA) patients are treated with celecoxib, ibuprofen or naproxen. Currently this trial has enrolled ~22,000 patients, who will be followed for 3 years.
-
-
Hypertension management is critical to lowering CV hazards.
-
What is also unclear is if rheumatologists should be screening our patients for CV risk using the Framingham risk calculator to identify the 10yr risk for CVE. Nonetheless, the predictive value of such calculations in RA has yet to be shown.
-
cIMT (carotid intima media thickening) is an increasingly used tool to measure vascular disease.
-
HDL: it’s not the level (higher did not protect) – it’s how well HDL functions. Mechanisms underlying dysfunctional HDL are not known, but are under investigation.
-
Abundant amounts of dysfunctional Apolipoprotein A1 are found in RA patients.
-
The “CIRT” trial is underway to prospectively study if MTX can be given reduce the risk of MI, CVA, CV death in non-RA patients with a prior MI history.
Dr. Carol Langford – Biologics and Vasculitis
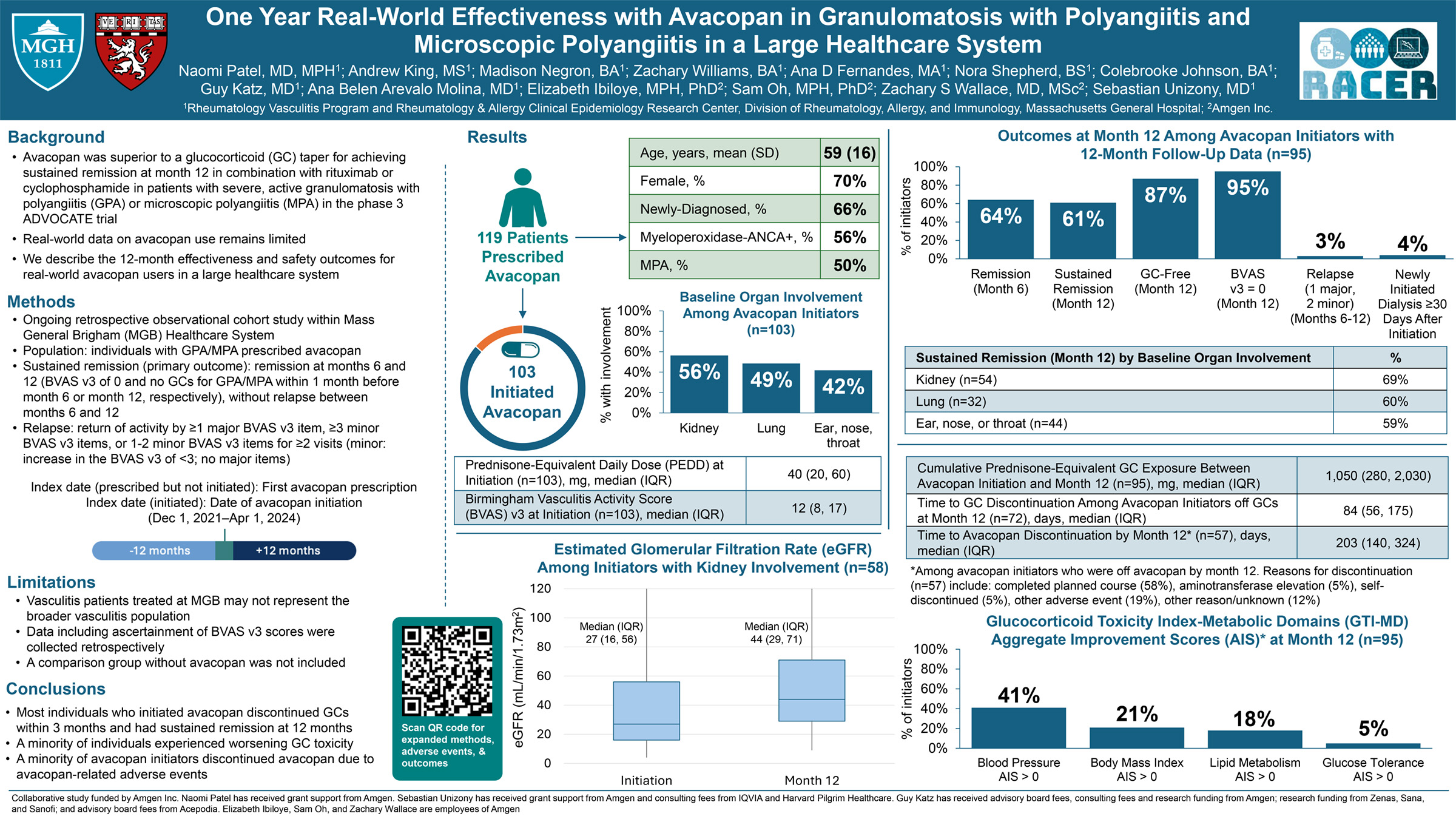
Dr. Langford reviewed the current status of vasculitis management in 2015 and the role that biologic therapies may play. She reviewed what is known about the use of biologics in disorders like GPA, EGPA, and large vessel vasculitis (GCA and Takayasu’s arteritis)
-
For severe Wegener’s/GPA, cyclophosphamide (CTX) and rituximab are the mainstays of induction therapy. Maintenance on MTX, azathioprine, mycophenolate or RTX is appropriate. For non-severe GPA, MTX has been effective.
-
WGET (etanercept in GPA/Wegener’s): showed the addition of a TNF inhibitor did not improve remission rates in GPA.
-
RAVE Trial (CTX vs RTX for remission induction in GPA or MPA): published in the NEJM 2010 showed that rituximab was equal to cyclophosphamide or prednisone; relapse rates were fewer in RTX.
-
There are not enough studies to prove that RTX should be the preferred drug in all populations of GPA.
-
Abatacept is being studied in GPA (ABROGATE trial) starting in 2015.
-
Anti-TNF therapies have not been shown to be effective in giant cell arteritis (GCA).
-
On the other hand 2 series showed that TNF inhibitor use did lower steroid use, the number of patients treated in these trials was very low.
-
-
IL-6 inhibition in large vessel vasculitis (GCA, Takayasu’s arteritis) is attracting more interest
-
Anti-IL6 treatment: efficacy is unknown but there are case reports demonstrating benefits in refractory patients with GCA or TAK or PMR. However, there are also 2 reports showing no benefit.
-
Enrollment in a large RCT has just completed so future data on IL-6 inhibition in GCA/TAK awaits.
-
-
There is no current role for abatacept as data is lacking. A trial of ABA in GCA or TAK has just completed enrollment.
-
B cell Depletion in GCA or TAK – early reports, but no studies are available to define a clear role for RTX.
-
Newly diagnosed GCA or TAK – there is no role for biologics. Steroids are the mainstay.
-
Hepatitis C Virus associated Cryoglobulinemic vasculitis: >80% of cryoglobulinemic vasculitis is related to HCV. Common findings include purpura, arthritis, neuropathy and glomerulonephritis.
-
RTX studied in 2 RCTs. The efficacy was so superior the studies were halted prematurely.
-
However, with this diagnosis being attributed to HCV – the best choice of treatment would be antiviral therapy that would eradicate the HCV.
-
Other options may include plasmapheresis (risk of thrombosis or infection) or B cell depletion.
-
-
Behcet’s: Ocular disease (panuveitis or AAU) is the most severe of manifestations and occurs in 25-75% of patients. Current treatment options include steroids, azathioprine, CTX, cyclosporine, mycophenolate and TNF inhibitors.
-
Apremilast recently shown in NEJM March 2015: noted less pain, fewer oral ulcers in 111 patients, mostly enrolled from Turkey > USA.
-
-
EGPA (Churg Strauss): Rx based on disease severity, asthma can be difficult to manage and make steroid reduction fraught with difficulty.
-
Retrospective report from 4 centers: 41 patients treated with RTX - remission seen in up to 49% @12 mos., with 83% improved by 6 mos. Steroid reduction was successful in all.
-
Novel treatment with anti-IL-5 (Mepolizumab): promising results have been seen in asthma and hypereosinophilic syndrome.
-
2 pilot studies showed open-label improvement in nearly all and flare when switched to MTX.
-
-