If You See Something, Say Something Save

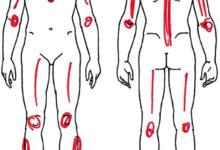
Just yesterday I saw an Ank-Spond, 2 RA, 2 hand OAs and a teenager with lupus.
No, I wasn’t in clinic. Instead I was making my way through the airport to the Amway Hotel in Grand Rapids and keenly spotted these pathognomonic diagnoses without any effort.
Surely, this happens to you too. Either you’re people watching, or in line at the store and you just can’t help but notice someone with an obvious, across-the-room diagnosis of something you specialize in?
Is it enough to be proud of your diagnostic prowess or should you be doing something with such observatory skills? Would you go up to an utter stranger and say, “excuse me sir, but did you know you have ankylosing spondylitis?”
I’ve asked this question to many rheumatologists – at lectures, privately or on twitter. And the response is unanimous, they admit it happens to them but they never confront the stranger with ankylosing spondylitis.
I have to admit I don’t blindly approach pretty women (for any reason) and hate being approached by strangers who begin with, “excuse me sir, can I ask you…”. I usually raise the halting hand, veer right and say “no habla ingles”. (I assume this is what the pretty woman would say to me if I approached her.)
Most assume that it would either be a medical-legal violation of privacy or in the least would be rude to engage a stranger in conversation about their ailment. After all, you may embarrass them and yourself in doing so. Obviously you ‘d be risking alarm and harm if you confronted someone (in the same manner) who was obese, pregnant or discolored with vitiligo. So it seems prudent to just keep quiet and to yourself and avoid the keen coding of the public at large.
I too, never use to say anything to the obvious diagnosis person. Then one day I saw a 40ish, African-American parking valet who had obvious AS – a stooped forward straight back, forward head tilt and a fused spine that exemplified by whole body visual turns. I thought why not?
My line went something like, “excuse me sir, I couldn’t help but notice your difficulty with your spine. I’m an arthritis doctor and I thought you should know I believe you have a condition called ankylosing spondylitis.” [This is where I paused to receive a rebuke, punch or look for more information].
Thankfully a pleasant conversation ensued. I explained that many people with AS don’t know their diagnosis and he was one of them. He asked questions and told me he had seen an orthopedist who thought he should see a spine specialist, but he never did.
Since then I’ve done this a few more times and been surprised to see that “the intrusion” was warmly received – even if it was an incorrect diagnosis. Most were thankful, the conversations were short and a few said thanks but no discussion was necessary. I did not give my business card but did give them my name.
If you researched this subject you would find the following unanimous results: 1) Nearly all physicians prefer to keep to themselves and avoid the risk of talking to strangers; 2) lawyers and advisors say you should avoid the interactions where your involvement was not requested or sought; and 3) the vast majority of patients and lay audiences would definitely want you to speak to them and offer a learned, professional medical opinion about their wellness.
To be warmly received, it has to be warmly delivered, with the person’s privacy respected. Hence, I would not approach someone in a crowd or amongst their coworkers. Also, I have to ask for their permission to comment on their apparent medical problem while informing them I’m an observant medical specialist with some potentially useful medical information.
Does your Hippocratic obligation mandate that you do your utmost with your medical skills? Most agree that you should lend assistance in a medical emergency. But where do you draw the line on what is emergent, urgent or serious? Should the dermatologist confront strangers with suspicious lesions or classic cutaneous findings? Would you not address a serious medical problem (i.e., a BP of 178/118) discovered during your rheumatology clinic evaluation?
Here are my justifications for why I (or you) may want to speak up, engage and inform the population at large with information that I am expert in:
- You are expert! (and have skills beyond most mortal men). Rheumatology is a visual discipline as much as any other, including dermatology. Strong visuals, pattern recognition and communication skills are the essential traits of great rheumatologists. These aren’t tools you only use Monday through Friday, 8-5pm.
- Hippocratic Oath. The first section of the oath states invokes a moral code for medical practitioners, “I will use treatment to help the sick according to my ability and judgment, but never with a view of injury and wrong-doing.” (Citation http://buff.ly/2eldM0G)
- Misdiagnosis: is rampant. You know this is true based on what patients have been told and diagnosed before they come to you for consultation. Misdiagnoses are the common product of self-diagnosis, PCPs, family physicians and OBGYN and those who think a positive lab result equates with a specific diagnosis. Every rheumatologist knows that the delivery of a knowledgeable diagnosis is usually received with appreciation.
- Not seeking medical care or evaluation – this usually results in non-diagnosis, self-diagnosis and symptom management by a wide array of characters and promising products.
- You should be aware of Dr. Atul Deodhars analysis of the prevalence of AS and spondyloarthritis wherein he shows the under-recognition of AS/SpA, that is, in fact, much more prevalent than RA (Citation http://buff.ly/2ewjThQ). So if the population ratio of SpA:RA is 2:1, then why is the usual rheumatology clinic ratio more like 1:2 or 1:3? There are many conditions like AS or SpA that are underdiagnosed or not addressed by medical practitioners and patients.
Try it. Think of it as an act of kindness or passing on the knowledge. You may help a stranger greatly.
- Ask for permission to comment on a medical issue and keep it private.
- Simply state what’s obvious to you, identifying yourself as an observant physician.
- Be prepared to write down the diagnosis you wish to bring to their attention.
- Suggest the patient see a rheumatologist near where they live. Suggesting another practitioner will keep your altruism badge shiny.
“If you see something, say something” is a branded slogan for New York City and the Department of Homeland security that is invoked to engage and protect the public from that which is recognized and seen by many. You could do your part for rheumatology.
Tell me why you won’t or don’t talk to strangers about a diagnosis that’s plain and obvious to you.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.